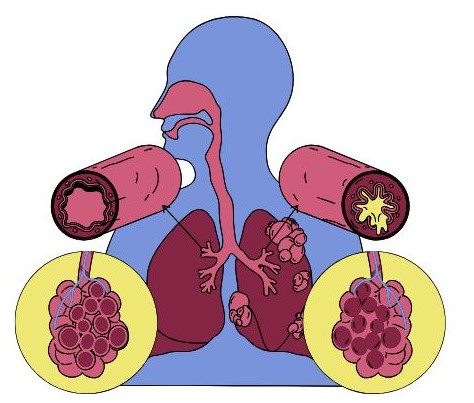
Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, making it difficult to breathe. It affects people of all ages but often starts in childhood. The exact cause of asthma is not fully understood, but it is thought to result from a combination of genetic and environmental factors.
Symptoms
- Shortness of Breath:
- This symptom may occur during physical activity or at rest, particularly when lying down. People with asthma often experience tightness in the chest, which contributes to the sensation of not being able to catch their breath.
- Wheezing:
- Wheezing is a high-pitched, whistling sound made while breathing, especially during exhalation. It occurs due to narrowed airways and can vary in intensity. Some may only wheeze during exertion, while others may wheeze at rest or during sleep.
- Coughing:
- The cough associated with asthma can be persistent and may worsen at night or early in the morning. It often occurs in response to cold air, exercise, or respiratory infections. Coughing can sometimes produce mucus, which may be thick and sticky.
- Chest Tightness or Pain:
- Individuals often describe a feeling of pressure or tightness in the chest. This discomfort can range from mild to severe and may be mistaken for a heart-related issue.
- Increased Mucus Production:
- Asthma can lead to an increase in mucus in the airways, which can contribute to coughing and wheezing. The mucus may become thick and difficult to clear.
- Difficulty Sleeping:
- Asthma symptoms can worsen at night, leading to disturbed sleep. Nocturnal asthma can be particularly challenging, causing nighttime awakenings due to coughing, wheezing, or shortness of breath.
- Fatigue:
- Frequent nighttime awakenings or ongoing symptoms can lead to daytime fatigue. Difficulty breathing can also drain energy levels, making it hard to maintain regular activities.
- Respiratory Infections:
- People with asthma may be more susceptible to respiratory infections, which can exacerbate asthma symptoms. Symptoms of infections, such as colds or the flu, can lead to increased wheezing, coughing, and difficulty breathing.
Variability of Symptoms
Asthma symptoms can vary significantly between individuals and may change over time. They can be:
- Intermittent: Occurring sporadically, often with periods of symptom-free intervals.
- Persistent: Symptoms occur regularly and may interfere with daily activities or sleep.
Triggered Symptoms
Asthma symptoms can be triggered by various factors, including:
- Allergens: Pollen, mold, pet dander, dust mites, and cockroach droppings.
- Irritants: Tobacco smoke, air pollution, strong odors (like perfumes), and chemical fumes.
- Exercise: Physical activity, particularly in cold, dry air.
- Weather Changes: Cold air, changes in humidity, and temperature fluctuations.
- Respiratory Infections: Colds, flu, and other viral infections can provoke symptoms.
- Emotional Stress: Strong emotions, including laughter, can trigger symptoms.
Monitoring Symptoms
Regular monitoring is essential for managing asthma. Individuals can track their symptoms using a journal or an app, noting frequency, severity, and any potential triggers. Peak flow meters can also help measure lung function and detect early signs of worsening asthma.
Understanding and recognizing the symptoms of asthma is crucial for effective management. Individuals experiencing asthma symptoms should work closely with healthcare providers to develop an action plan tailored to their specific needs, ensuring timely intervention and reducing the risk of severe asthma attacks.
Types of Asthma
- Allergic (Extrinsic) Asthma
- Characteristics: This type is triggered by allergens and is often associated with other allergic conditions like hay fever (allergic rhinitis) and eczema.
- Common Triggers: Pollen, mold spores, pet dander, dust mites, and cockroach droppings.
- Age of Onset: Typically develops in childhood or adolescence, but it can occur at any age.
- Non-Allergic (Intrinsic) Asthma
- Characteristics: This form is not related to specific allergens and may be triggered by non-allergic factors. It often has a more adult onset.
- Common Triggers: Stress, exercise, cold air, respiratory infections, strong odors, and smoke.
- Age of Onset: More common in adults, especially those who do not have a history of allergies.
- Exercise-Induced Asthma (EIA)
- Characteristics: Symptoms occur during or after physical activity. It’s often triggered by prolonged exertion, especially in cold, dry air.
- Common Triggers: Running, vigorous sports, or activities in cold environments.
- Symptoms: Wheezing, coughing, shortness of breath, and chest tightness during or after exercise.
- Occupational Asthma
- Characteristics: This type is triggered by exposure to allergens or irritants in the workplace. Symptoms may improve when away from work.
- Common Triggers: Chemicals, dust, fumes, or allergens specific to certain professions (e.g., flour dust in bakers, latex in healthcare workers).
- Symptoms: Similar to other types of asthma but often linked to work environments.
- Nocturnal Asthma
- Characteristics: Symptoms worsen at night, disrupting sleep. It can affect the quality of life and daily functioning.
- Common Triggers: Allergens in the bedroom (like dust mites), changes in temperature, or lying flat.
- Symptoms: Nighttime coughing, wheezing, and shortness of breath, often leading to waking up from sleep.
- Cough-Variant Asthma
- Characteristics: The primary symptom is a persistent cough, without the classic wheezing or shortness of breath. It can be misdiagnosed as a chronic cough.
- Common Triggers: Cold air, exercise, respiratory infections, and allergens.
- Symptoms: A dry, persistent cough that may worsen at night or during physical activity.
- Severe Asthma
- Characteristics: This type includes asthma that is difficult to control and may require high doses of medication or multiple medications. It can lead to frequent hospitalizations.
- Common Triggers: A combination of allergens, irritants, respiratory infections, and non-compliance with treatment.
- Symptoms: Frequent and severe symptoms that interfere with daily activities and may require emergency interventions.
Asthma Classification by Severity
In addition to the types, asthma can also be classified by severity, which is important for management:
- Mild Intermittent: Symptoms occur less than twice a week; nighttime symptoms occur less than twice a month.
- Mild Persistent: Symptoms occur more than twice a week but not daily; nighttime symptoms occur 3-4 times a month.
- Moderate Persistent: Daily symptoms; nighttime symptoms occur more than once a week but not nightly.
- Severe Persistent: Symptoms occur throughout the day on most days; frequent nighttime symptoms.
Understanding the different types of asthma is crucial for effective management and treatment. Each type may have unique triggers and symptoms, which can influence treatment approaches. Collaborating with a healthcare provider to develop a personalized management plan is essential for optimizing asthma control and improving quality of life.
Causes and Risk Factors
While the exact cause of asthma is not fully understood, several biological and environmental factors contribute to its development:
- Genetic Factors:
- Family History: A family history of asthma or allergies increases the likelihood of developing asthma. Certain genes may predispose individuals to hypersensitivity to allergens and airway inflammation.
- Immune System: An individual’s immune response to allergens may also have a genetic component, influencing how the body reacts to environmental triggers.
- Environmental Factors:
- Allergens: Exposure to allergens like pollen, mold, dust mites, and pet dander is a significant trigger for asthma symptoms, particularly in allergic (extrinsic) asthma.
- Irritants: Tobacco smoke, air pollution, chemical fumes, and strong odors can irritate the airways and trigger asthma attacks.
- Respiratory Infections:
- Viral Infections: Respiratory infections during infancy and early childhood, particularly viral infections like respiratory syncytial virus (RSV), can increase the risk of developing asthma.
- Inflammation: Infections can lead to chronic airway inflammation, which may contribute to asthma development later in life.
- Obesity:
- Excess weight is associated with increased inflammation in the body and can exacerbate asthma symptoms. Fat tissue can produce inflammatory chemicals that worsen airway responsiveness.
- Exercise:
- For some individuals, physical activity, especially in cold, dry air, can trigger asthma symptoms, leading to exercise-induced bronchoconstriction.
- Gastroesophageal Reflux Disease (GERD):
- GERD can exacerbate asthma symptoms, as acid reflux can irritate the airways, leading to coughing and wheezing.
Risk Factors for Asthma
Several factors increase the risk of developing asthma, including:
- Age:
- Asthma often begins in childhood, but it can develop at any age. Early exposure to allergens and respiratory infections can increase risk in children.
- Allergies:
- Individuals with a history of allergies, such as hay fever, eczema, or food allergies, are more likely to develop asthma. The immune system’s response to allergens can lead to airway hyperreactivity.
- Exposure to Tobacco Smoke:
- Prenatal exposure to tobacco smoke and secondhand smoke exposure in childhood are strong risk factors for asthma. Smoke can irritate the airways and contribute to inflammation.
- Air Pollution:
- Exposure to outdoor air pollutants, such as vehicle emissions and industrial pollutants, is linked to an increased risk of asthma, particularly in urban areas.
- Occupational Exposures:
- Certain occupations expose individuals to allergens or irritants, increasing the risk of occupational asthma. Jobs in industries like healthcare, manufacturing, and agriculture are commonly associated with this risk.
- Stress:
- Emotional stress and anxiety can exacerbate asthma symptoms. Stress can affect breathing patterns and airway function, leading to increased sensitivity.
- Geographic Location:
- Living in areas with high pollen counts or significant air pollution can increase asthma risk. Weather conditions and seasonal variations also play a role in symptom exacerbation.
- Socioeconomic Status:
- Individuals from lower socioeconomic backgrounds may have increased exposure to environmental triggers (like poor housing conditions) and reduced access to healthcare, leading to worse asthma outcomes.
Asthma is a multifactorial condition influenced by a combination of genetic, environmental, and lifestyle factors. Understanding these causes and risk factors can help individuals and healthcare providers identify potential triggers and implement strategies for prevention and management. Early intervention and education are crucial in minimizing the impact of asthma on daily life. If you have concerns about asthma, consulting a healthcare professional for a personalized assessment and management plan is essential.
Diagnosis of Asthma
- Medical History:
- Symptom Review: The healthcare provider will ask about the frequency, duration, and severity of symptoms such as coughing, wheezing, shortness of breath, and chest tightness.
- Trigger Identification: Patients will be asked to identify potential triggers, including allergens, irritants, physical activity, and emotional stress.
- Family History: A family history of asthma, allergies, or other respiratory conditions can provide important context.
- Physical Examination:
- Breathing Assessment: The healthcare provider will listen to the patient’s lungs using a stethoscope to check for wheezing or other abnormal sounds.
- General Health Check: Examination for signs of allergic conditions (e.g., nasal polyps, eczema) may also be conducted.
- Lung Function Tests:
- Spirometry: This is the most common test used to assess lung function. The patient will be asked to take a deep breath and then exhale forcefully into a spirometer, which measures:
- Forced Vital Capacity (FVC): The total amount of air exhaled forcefully after taking a deep breath.
- Forced Expiratory Volume in 1 Second (FEV1): The amount of air exhaled in the first second of the forced exhalation.
- A reduced FEV1/FVC ratio indicates airway obstruction, which is characteristic of asthma.
- Reversibility Testing: After spirometry, the patient may be given a bronchodilator (a quick-relief inhaler) to see if lung function improves. An increase in FEV1 of 12% or more after medication suggests asthma.
- Spirometry: This is the most common test used to assess lung function. The patient will be asked to take a deep breath and then exhale forcefully into a spirometer, which measures:
- Peak Flow Monitoring:
- Peak Expiratory Flow Rate (PEFR): Patients may be instructed to use a peak flow meter at home to measure their maximum speed of expiration. This can help track asthma control over time.
- Bronchial Provocation Tests:
- Methacholine Challenge: In this test, the patient inhales increasing doses of methacholine, a substance that can trigger asthma symptoms. If the patient experiences a significant drop in lung function, it indicates airway hyperreactivity.
- Exercise Challenge: This test assesses exercise-induced asthma by measuring lung function before and after exercise.
- Allergy Testing:
- Skin Prick Tests: This involves applying small amounts of allergens to the skin to see if a reaction occurs, indicating allergies that may trigger asthma.
- Blood Tests: Specific IgE tests can measure the immune response to particular allergens, helping identify potential triggers.
- Imaging Tests:
- Chest X-ray: While not routinely used for asthma diagnosis, a chest X-ray can help rule out other conditions, such as infections or structural abnormalities in the lungs.
- Differential Diagnosis:
- Healthcare providers will consider other conditions that may mimic asthma symptoms, such as chronic obstructive pulmonary disease (COPD), vocal cord dysfunction, or gastroesophageal reflux disease (GERD).
- Asthma Control Assessment:
- Tools like the Asthma Control Test (ACT) or the Asthma Control Questionnaire (ACQ) may be used to evaluate how well asthma is being managed and its impact on daily life.
The diagnosis of asthma is a comprehensive process that involves understanding the patient’s medical history, conducting physical examinations, and utilizing various tests to assess lung function and identify triggers. Early and accurate diagnosis is crucial for effective management and treatment, helping to reduce symptoms and improve the quality of life for individuals with asthma. If you suspect you have asthma, it’s essential to consult a healthcare provider for a thorough evaluation and personalized management plan.
Management and Treatment
1. Medication Management
a. Long-Term Control Medications These medications are taken daily to maintain asthma control and prevent symptoms.
- Inhaled Corticosteroids (ICS):
- Examples: Fluticasone, budesonide, beclomethasone.
- Function: Reduce inflammation in the airways, decreasing the frequency and severity of asthma attacks.
- Long-Acting Beta Agonists (LABAs):
- Examples: Salmeterol, formoterol.
- Function: Relax the muscles around the airways for up to 12 hours. LABAs are typically used in combination with ICS.
- Leukotriene Modifiers:
- Examples: Montelukast, zafirlukast.
- Function: Block leukotrienes, which are chemicals in the immune system that cause airway constriction and inflammation.
- Theophylline:
- Function: A bronchodilator that relaxes the airways, improving airflow. It requires regular monitoring due to potential side effects.
- Biologics:
- Examples: Omalizumab, mepolizumab, benralizumab.
- Function: Target specific pathways in asthma (e.g., IgE levels or eosinophils) and are used for severe asthma that is difficult to control.
b. Quick-Relief (Rescue) Medications These medications are used for immediate relief during asthma attacks.
- Short-Acting Beta Agonists (SABAs):
- Examples: Albuterol, levalbuterol.
- Function: Provide rapid bronchodilation, relieving acute symptoms within minutes.
- Anticholinergics:
- Example: Ipratropium bromide.
- Function: Can be used in combination with SABAs for additional relief, particularly in severe attacks.
2. Asthma Action Plan
- Personalized Plan: A written asthma action plan developed with a healthcare provider outlines daily management strategies and instructions for responding to worsening symptoms.
- Monitoring: The plan includes instructions on how to monitor symptoms and peak flow readings to assess control and recognize early signs of an asthma attack.
3. Avoiding Triggers
Identifying and minimizing exposure to triggers is essential for effective asthma management:
- Allergen Management:
- Use dust mite covers on pillows and mattresses, maintain low indoor humidity, and keep pets out of sleeping areas.
- Irritant Avoidance:
- Avoid tobacco smoke, strong odors, and pollutants. Use air purifiers if necessary.
- Weather and Exercise Management:
- Be cautious with outdoor activities during high pollen seasons or cold weather. Pre-medicate with a SABA before exercise if exercise-induced symptoms are common.
4. Lifestyle Modifications
- Healthy Diet:
- A balanced diet rich in fruits, vegetables, and omega-3 fatty acids can support overall health and potentially reduce inflammation.
- Weight Management:
- Maintaining a healthy weight can improve asthma control, as excess weight can exacerbate symptoms.
- Regular Exercise:
- Engage in regular, moderate exercise as tolerated. Activities like swimming may be beneficial since the warm, moist air can be less irritating to the airways.
- Stress Management:
- Techniques such as yoga, meditation, and breathing exercises can help manage stress, which can trigger asthma symptoms.
5. Regular Medical Follow-Up
- Routine Check-Ups: Regular visits to a healthcare provider are essential to monitor asthma control, adjust medications, and ensure adherence to the asthma action plan.
- Education: Patients and caregivers should receive ongoing education about asthma management, including proper inhaler technique and recognizing symptoms of worsening asthma.
6. Emergency Preparedness
- Recognizing Severe Symptoms: Educating patients on recognizing when asthma symptoms become severe and when to seek emergency care is crucial.
- Emergency Medications: Ensure quick-relief medications are always accessible, particularly during travel or physical activity.
Effective asthma management requires a multifaceted approach that includes medication, trigger avoidance, lifestyle modifications, regular monitoring, and education. By working closely with healthcare providers to develop a personalized asthma action plan and adhering to treatment, individuals with asthma can lead healthy, active lives. If you or someone you know is struggling with asthma, it’s important to consult a healthcare provider for tailored advice and support.
Asthma and COVID-19: understanding the Connection
1. Risk of Severe Illness
- General Findings: Initial studies suggested that people with asthma may be at higher risk for severe outcomes if they contract COVID-19. However, further research indicates that the risk may vary depending on the severity of asthma and individual health factors.
- Controlled vs. Uncontrolled Asthma: Individuals with well-managed asthma, particularly those whose symptoms are mild or intermittent, may not have a significantly increased risk. In contrast, those with severe or uncontrolled asthma may face a greater risk of complications.
2. Asthma Medications and Immune Response
- Inhaled Corticosteroids: Many people with asthma use inhaled corticosteroids, which reduce airway inflammation. Some research suggests that these medications may have a protective effect against severe COVID-19 outcomes by modulating the immune response.
- Bronchodilators: Short-acting beta agonists (SABAs) are commonly used as rescue inhalers and do not appear to negatively affect COVID-19 outcomes. There is no evidence suggesting that they increase the risk of infection or worsen severity.
3. Asthma Symptoms and COVID-19
- Overlap of Symptoms: Symptoms of asthma, such as coughing and shortness of breath, can overlap with symptoms of COVID-19, making it challenging to distinguish between the two. This can lead to anxiety and the need for testing during the pandemic.
- Increased Respiratory Infections: Individuals with asthma may have a higher susceptibility to respiratory infections, which could increase the risk of contracting COVID-19 or experiencing complications.
4. Precautions for Individuals with Asthma
- Vaccine Recommendations: Public health authorities recommend COVID-19 vaccination for individuals with asthma, as vaccines have been shown to reduce the risk of severe illness, hospitalization, and death. Vaccination is particularly important for those with uncontrolled or severe asthma.
- Continued Asthma Management: It’s crucial for individuals with asthma to adhere to their prescribed asthma management plan, including taking medications as directed and avoiding triggers.
5. Long COVID and Asthma
- Long COVID: Some individuals who recover from COVID-19 may experience lingering symptoms, known as long COVID. For individuals with asthma, this could mean an exacerbation of asthma symptoms or new respiratory issues.
- Research Gaps: Ongoing research is needed to fully understand the implications of COVID-19 on individuals with asthma, particularly regarding long-term effects and how to best manage any new or worsening symptoms.
6. Mental Health Considerations
- Anxiety and Stress: The pandemic has heightened anxiety and stress for many, including those with asthma. Increased stress can exacerbate asthma symptoms, creating a cyclical problem. It’s essential for individuals to engage in stress-reduction techniques and seek mental health support if needed.
While there are concerns about COVID-19 for individuals with asthma, particularly those with severe or uncontrolled forms, many people with well-managed asthma do not appear to be at significantly increased risk for severe illness. Vaccination and adherence to asthma management plans remain vital. Individuals should stay informed about emerging research and continue to consult healthcare providers to optimize their asthma care during and after the pandemic.

Asthma is a prevalent respiratory condition that requires careful management and understanding. By recognizing triggers, adhering to treatment plans, and making necessary lifestyle changes, individuals with asthma can lead healthy and active lives. Ongoing research continues to improve our understanding of the disease and its management, offering hope for better outcomes for those affected.