What is Celiac Disease? A comprehensive Explanation
Celiac disease is a chronic autoimmune disorder characterized by an inappropriate immune response to gluten, a protein found in wheat, barley, and rye. When individuals with celiac disease consume gluten, their immune system mistakenly attacks the lining of the small intestine, leading to inflammation and damage.
Mechanism of Celiac Disease
- Immune Response: In genetically predisposed individuals, gluten triggers the immune system to produce antibodies against the protein. This immune response primarily targets an enzyme called tissue transglutaminase (tTG), which is involved in processing gluten.
- Intestinal Damage: The immune reaction leads to inflammation and the destruction of the villi—small finger-like projections in the small intestine that are crucial for nutrient absorption. As a result, the surface area of the intestine is reduced, leading to malabsorption of nutrients.
- Genetic Factors: Celiac disease is strongly associated with certain genetic markers. The majority of affected individuals carry either the HLA-DQ2 or HLA-DQ8 gene. However, carrying these genes does not guarantee the development of the disease; it requires the presence of additional environmental triggers.
Environmental Triggers
While genetic predisposition is vital, various environmental factors may trigger celiac disease in susceptible individuals, including:
Dietary Changes: Introduction of gluten into the diet at a young age can also influence the likelihood of developing celiac disease.
Gluten Exposure: Consuming gluten-containing foods is the most direct trigger.
Infections: Certain gastrointestinal infections may precipitate the onset of symptoms in genetically predisposed individuals.
Symptoms of Celiac Disease
Celiac disease can manifest with a wide range of symptoms that vary in severity and presentation. Some individuals may experience primarily gastrointestinal symptoms, while others may have non-gastrointestinal symptoms. Here’s a detailed look at the various symptoms associated with celiac disease:
Gastrointestinal Symptoms
- Chronic Diarrhea:
- Frequent, watery stools are common, often accompanied by urgency.
- Constipation:
- Some individuals may experience persistent constipation instead of diarrhea.
- Abdominal Pain:
- Cramping or sharp pain in the abdomen, often accompanied by bloating.
- Bloating and Gas:
- A feeling of fullness and distention in the abdomen, often with excessive gas production.
- Nausea and Vomiting:
- Some people may experience feelings of nausea, leading to vomiting in some cases.
- Fatty Stools (Steatorrhea):
- Stools may appear pale, foul-smelling, and greasy due to unabsorbed fat.
Non-Gastrointestinal Symptoms
- Fatigue:
- Chronic tiredness is common, often related to malabsorption of nutrients.
- Weight Loss or Failure to Thrive:
- Unintentional weight loss in adults or delayed growth in children due to nutrient deficiencies.
- Nutritional Deficiencies:
- Deficiencies in iron (leading to anemia), calcium (affecting bone health), and vitamins (like B12 and D) can occur.
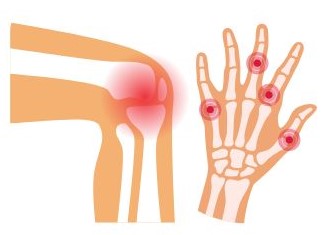
- Dermatitis Herpetiformis:
- An itchy, blistering skin rash that typically appears on the elbows, knees, and buttocks. This condition is directly linked to gluten ingestion.
- Bone or Joint Pain:
- Chronic pain in bones or joints may result from osteoporosis or other related conditions.
- Neurological Symptoms:
- Issues such as headaches, migraines, numbness, or tingling in the hands and feet (peripheral neuropathy) can occur.
- Mood Disorders:
- Anxiety, depression, and mood swings are frequently reported, potentially linked to nutrient deficiencies or the psychological impact of living with the disease.
- Reproductive Issues:
- Women may experience irregular menstrual cycles, infertility, or complications during pregnancy.
- Dental Enamel Defects:
- Changes in tooth enamel, such as discoloration or pitting, may be evident, often noted during dental check-ups.
- Delayed Growth and Development in Children:
- Children may experience stunted growth, delayed puberty, and behavioral issues.
Variability of Symptoms
It’s important to note that symptoms can vary widely between individuals. Some may have only mild symptoms, while others may experience severe manifestations. Moreover, the onset of symptoms can occur shortly after gluten consumption or may develop gradually over time.
Asymptomatic Cases
Interestingly, some individuals with celiac disease may remain asymptomatic or have very few symptoms. This can lead to underdiagnosis, as they might not seek medical attention. Even in the absence of symptoms, ongoing intestinal damage can still occur.
Celiac disease presents a complex array of symptoms, affecting various systems in the body. This variability can make diagnosis challenging, often requiring a thorough medical evaluation. If you suspect you or someone you know may have celiac disease, it’s crucial to consult a healthcare professional for appropriate testing and management. Early diagnosis and adherence to a gluten-free diet can significantly improve quality of life and prevent long-term complications.
Diagnosis of Celiac Disease
Diagnosing celiac disease involves a multi-step process that includes clinical evaluation, laboratory testing, and sometimes endoscopic examination. Here’s an in-depth look at each component of the diagnostic process:
1. Clinical Evaluation
- Medical History:
- Physicians begin by taking a comprehensive medical history, including any gastrointestinal symptoms (e.g., diarrhea, bloating), nutritional deficiencies, and family history of celiac disease or other autoimmune disorders.
- Symptom Assessment:
- A detailed assessment of current symptoms, duration, and severity is crucial. Doctors may inquire about the onset of symptoms in relation to gluten intake.
2. Blood Tests
Serological tests are critical for initial diagnosis. Common tests include:
- Anti-Tissue Transglutaminase Antibodies (tTG-IgA):
- This is the most commonly used screening test. Elevated levels of tTG-IgA antibodies indicate an immune response to gluten.
- Anti-Endomysial Antibodies (EMA):
- This test is highly specific for celiac disease but less commonly used due to its higher cost. A positive EMA test supports the diagnosis.
- Deamidated Gliadin Peptide (DGP) Antibodies:
- This test can be helpful, especially in children or in cases where tTG-IgA levels are normal.
- Total IgA Levels:
- Since some individuals may have IgA deficiency, measuring total IgA levels ensures that the other tests are interpreted correctly. In cases of IgA deficiency, IgG-based tests may be used.
3. Endoscopy and Biopsy
If blood tests suggest celiac disease, the next step is often an endoscopy:
- Upper Endoscopy:
- A thin, flexible tube with a camera is inserted through the mouth and into the small intestine. This allows for direct visualization of the intestinal lining.
- Biopsy:
- During the endoscopy, small tissue samples (biopsies) are taken from the duodenum (the first part of the small intestine). A pathologist examines these samples for:
- Villous Atrophy: Damage to the villi, which are small finger-like projections that absorb nutrients.
- Intraepithelial Lymphocytes: An increased number of immune cells can indicate an inflammatory response.
- During the endoscopy, small tissue samples (biopsies) are taken from the duodenum (the first part of the small intestine). A pathologist examines these samples for:
4. Genetic Testing
While not required for diagnosis, genetic testing can be beneficial in certain scenarios:
- HLA-DQ2 and HLA-DQ8 Testing:
- Testing for these specific genetic markers helps confirm susceptibility to celiac disease. However, the presence of these genes alone is not sufficient for diagnosis, as many people carry them without developing the disease.
5. Differential Diagnosis
It’s essential to rule out other conditions that can cause similar symptoms, such as:
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease (IBD)
- Lactose Intolerance
- Food Allergies
- Other Autoimmune Disorders
6. Follow-Up Testing
Once diagnosed, follow-up tests may include:
- Repeat Serological Testing:
- After starting a gluten-free diet, doctors may monitor antibody levels to ensure they decrease and to assess adherence to the diet.
- Nutritional Assessments:
- Evaluating for nutritional deficiencies (e.g., iron, calcium, vitamins) and addressing any issues through dietary changes or supplementation.
Diagnosing celiac disease is a comprehensive process that involves careful clinical assessment, blood testing, and sometimes endoscopic evaluation. A thorough understanding of the diagnostic criteria and methods is crucial for effective identification and management of the condition. If you suspect celiac disease, seeking evaluation from a healthcare professional with experience in this area is vital for accurate diagnosis and timely intervention.
Treatment of Celiac Disease
The primary and most effective treatment for celiac disease is a strict gluten-free diet. This approach is essential for managing symptoms, promoting intestinal healing, and preventing long-term complications. Here’s a detailed overview of treatment options and management strategies.
1. Gluten-Free Diet
Fundamentals:
- The gluten-free diet involves eliminating all sources of gluten from the diet. This includes foods and ingredients derived from wheat, barley, and rye.
Food Sources to Avoid:
- Wheat Products: Bread, pasta, cereals, baked goods, and many processed foods.
- Barley and Rye: Beer, malt, and other products made from these grains.
- Processed Foods: Many packaged foods may contain gluten as a thickener or stabilizer, requiring careful label reading.
Safe Food Alternatives:
- Naturally Gluten-Free Grains: Rice, corn, quinoa, millet, and buckwheat.
- Fruits and Vegetables: All fresh fruits and vegetables are gluten-free.
- Meat and Dairy: Fresh meats, fish, eggs, and dairy products are generally safe.
- Legumes and Nuts: Beans, lentils, and most nuts are gluten-free.
- Gluten-Free Products: Many brands offer gluten-free versions of common foods (breads, pastas, snacks).
2. Nutritional Support
- Dietitian Consultation: Working with a registered dietitian experienced in celiac disease can help individuals understand food choices, read labels, and create balanced meal plans.
- Nutritional Supplements: If deficiencies are present, supplements may be recommended. Common deficiencies include iron, calcium, vitamin D, and vitamin B12.
3. Monitoring and Follow-Up
- Regular Check-Ups: Follow-up appointments with healthcare providers are essential to monitor health, assess adherence to the diet, and evaluate for any nutritional deficiencies.
- Serological Testing: After implementing a gluten-free diet, blood tests are often repeated to check antibody levels, confirming adherence and improvement.
4. Management of Complications
- Bone Health: Since celiac disease can lead to osteoporosis, individuals should monitor bone density and may need calcium and vitamin D supplementation.
- Dermatitis Herpetiformis Treatment: Those with this skin condition may require specific treatments, such as dapsone, in addition to a gluten-free diet.
5. Lifestyle and Behavioral Considerations
- Education and Support: Joining support groups and connecting with others who have celiac disease can provide emotional support and practical tips for living gluten-free.
- Cross-Contamination Awareness: Understanding how to prevent cross-contact in the kitchen and during food preparation is crucial. This includes using separate utensils, toasters, and cooking surfaces for gluten-free foods.
6. Ongoing Research and Future Treatments
While the gluten-free diet is the current standard treatment, ongoing research is exploring additional therapeutic options, such as:
- Enzyme Supplements: Research is underway on enzymes that could potentially break down gluten in the digestive tract, but these are not yet widely available or proven effective.
- Vaccines: Investigations into vaccines that might help the immune system tolerate gluten are in progress, although these are still in experimental stages.
Managing celiac disease primarily involves adhering to a strict gluten-free diet, which can lead to significant improvement in symptoms and quality of life. With proper guidance, education, and support, individuals with celiac disease can lead healthy, fulfilling lives. Regular follow-up care and monitoring for complications are essential for long-term health. If you suspect celiac disease or have been diagnosed, working closely with healthcare professionals will provide the best outcomes.
Long-Term Complications of Celiac Disease
If left untreated, celiac disease can lead to various long-term complications due to ongoing damage to the small intestine and malabsorption of nutrients. Here’s a detailed overview of potential complications associated with celiac disease:
1. Nutritional Deficiencies
Due to the malabsorption caused by intestinal damage, individuals with untreated celiac disease often face deficiencies in several essential nutrients, including:
- Iron: Can lead to iron-deficiency anemia, resulting in fatigue, weakness, and pale skin.
- Calcium and Vitamin D: Increased risk of osteoporosis or osteopenia, leading to weakened bones and a higher likelihood of fractures.
- Vitamin B12: Deficiency can cause neurological symptoms, such as numbness, tingling, and cognitive issues.
- Folate: Low levels can contribute to anemia and complications during pregnancy.
2. Osteoporosis
The risk of developing osteoporosis is significantly higher in individuals with celiac disease due to malabsorption of calcium and vitamin D. This can lead to:
- Increased bone fragility.
- A higher risk of fractures, especially in older adults.
3. Intestinal Lymphoma
Celiac disease increases the risk of certain types of cancer, particularly:
- Enteropathy-Associated T-cell Lymphoma (EATL): A rare form of cancer that can develop in the small intestine due to chronic inflammation from untreated celiac disease.
While the overall risk is still low, the likelihood increases significantly in those who remain on a gluten-containing diet.
4. Other Gastrointestinal Disorders
Individuals with celiac disease may also be at higher risk for developing:
- Irritable Bowel Syndrome (IBS): Some people experience IBS-like symptoms, which can complicate diagnosis and management.
- Small Intestinal Bacterial Overgrowth (SIBO): Malabsorption can lead to changes in gut flora, increasing the risk of bacterial overgrowth.
5. Autoimmune Disorders
Celiac disease is associated with an increased risk of other autoimmune conditions, including:
- Type 1 Diabetes: The risk of developing type 1 diabetes is higher in individuals with celiac disease and vice versa.
- Thyroid Disorders: Conditions such as Hashimoto’s thyroiditis and Graves’ disease are more common in those with celiac disease.
- Liver Disease: Conditions such as autoimmune hepatitis can occur in conjunction with celiac disease.
6. Reproductive Health Issues
Untreated celiac disease can lead to various reproductive health complications, including:
- Infertility: Women may experience difficulty conceiving, and men may face reduced fertility due to hormonal imbalances.
- Pregnancy Complications: Increased risk of miscarriage, preterm birth, low birth weight, and complications related to nutrient deficiencies.
7. Neurological Issues
Some individuals with celiac disease may experience neurological complications, such as:
- Peripheral Neuropathy: Tingling, numbness, or pain in the extremities due to nerve damage.
- Ataxia: Loss of coordination and balance, which can be debilitating.
8. Psychological Impact
Living with celiac disease can also have psychological effects, including:
- Anxiety and Depression: The stress of managing a lifelong dietary restriction and potential social challenges can contribute to mental health issues.
- Quality of Life: Chronic health conditions can affect overall quality of life, leading to isolation or difficulties in social situations.
Long-term complications of untreated celiac disease underscore the importance of adhering to a strict gluten-free diet. Early diagnosis and appropriate management can significantly reduce the risk of these complications and improve quality of life. Regular follow-ups with healthcare providers are essential for monitoring health and addressing any issues related to nutritional deficiencies or related conditions. If you have celiac disease, maintaining awareness of potential complications and seeking proactive care is vital for long-term health.

Celiac disease is a serious autoimmune condition that requires lifelong management through a strict gluten-free diet. Awareness and education about the disease are crucial for proper diagnosis and management. As research continues, better understanding of celiac disease’s complexities will hopefully lead to improved treatment options and support for those affected. If you suspect you or a loved one may have celiac disease, consult a healthcare professional for evaluation and testing.