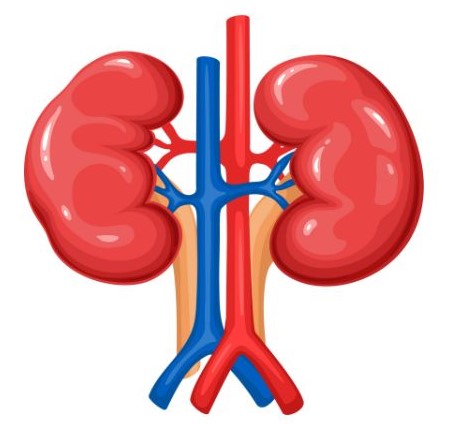
Kidney disease refers to a range of conditions that affect kidney function, leading to the kidneys’ inability to filter waste products and excess fluids from the blood effectively. The kidneys are vital organs that play essential roles in regulating blood pressure, electrolyte balance, and red blood cell production, among other functions.
Types of Kidney Disease
- Chronic Kidney Disease (CKD):
- Description: A gradual loss of kidney function over time, often due to long-term conditions such as diabetes or hypertension.
- Stages: CKD is classified into five stages based on the glomerular filtration rate (GFR), with Stage 1 being mild and Stage 5 indicating kidney failure.
- Acute Kidney Injury (AKI):
- Description: A sudden decline in kidney function, often reversible. It can occur due to factors like dehydration, medications, or severe infections.
- Causes: Includes reduced blood flow to the kidneys, direct damage to the kidneys, or urinary obstruction.
- Kidney Stones:
- Description: Hard deposits made of minerals and salts that form inside the kidneys, causing pain and potentially obstructing urine flow.
- Types: Calcium stones, uric acid stones, struvite stones, and cystine stones.
- Glomerulonephritis:
- Description: Inflammation of the kidney’s filtering units (glomeruli), which can lead to kidney damage. It can be acute or chronic.
- Causes: Infections, autoimmune diseases, and certain medications.
- Polycystic Kidney Disease (PKD):
- Description: A genetic disorder characterized by the formation of multiple cysts in the kidneys, leading to kidney enlargement and dysfunction.
- Types: Autosomal dominant (more common) and autosomal recessive (rare).
- Diabetic Nephropathy:
- Description: Kidney damage resulting from diabetes, often leading to CKD.
- Pathophysiology: High blood sugar levels cause damage to the kidneys’ filtering system over time.
Causes and Risk Factors
- Diabetes:
- Description: High blood sugar levels from uncontrolled diabetes can damage the kidneys’ filtering units (nephrons). This damage can progress to diabetic nephropathy, a leading cause of chronic kidney disease (CKD).
- Mechanism: Elevated glucose levels lead to increased pressure in the kidney’s blood vessels, causing scarring and reduced kidney function over time.
- Hypertension (High Blood Pressure):
- Description: Chronic high blood pressure can cause blood vessels in the kidneys to thicken and narrow, reducing blood flow and kidney function.
- Mechanism: Increased pressure can damage the glomeruli, the filtering units of the kidneys, leading to CKD.
- Glomerulonephritis:
- Description: Inflammation of the kidney’s filtering units can result from infections, autoimmune diseases, or other conditions. It can be acute or chronic.
- Causes: Conditions like lupus, IgA nephropathy, and post-infectious glomerulonephritis.
- Polycystic Kidney Disease (PKD):
- Description: A genetic disorder characterized by the growth of numerous cysts in the kidneys, leading to enlarged kidneys and decreased function.
- Inheritance: Autosomal dominant PKD is the most common form, and symptoms often appear in adulthood.
- Kidney Stones:
- Description: Hard deposits of minerals and salts that form in the kidneys, which can cause pain and obstruction.
- Risk Factors: Dehydration, certain dietary factors (high sodium, low calcium), and metabolic disorders.
- Obstructive Uropathy:
- Description: Blockage of the urinary tract that prevents urine from draining out of the kidneys, leading to kidney damage.
- Causes: Conditions like enlarged prostate, kidney stones, or tumors can cause obstruction.
- Infections:
- Description: Recurrent urinary tract infections (UTIs) or kidney infections (pyelonephritis) can damage kidney tissues.
- Chronicity: Frequent infections can lead to scarring and chronic kidney damage.
- Autoimmune Diseases:
- Description: Conditions in which the immune system attacks the body’s own tissues, including the kidneys.
- Examples: Systemic lupus erythematosus (SLE) and vasculitis.
- Medications and Toxins:
- Description: Certain medications can cause kidney damage, particularly when used long-term or in high doses.
- Examples: Non-steroidal anti-inflammatory drugs (NSAIDs), some antibiotics, and certain contrast dyes used in imaging tests.
- Cardiovascular Diseases:
- Description: Heart conditions can affect kidney function due to the interconnected nature of cardiovascular and renal systems.
- Mechanism: Poor blood flow to the kidneys can lead to decreased filtration and kidney injury.
Risk Factors for Kidney Disease
- Age:
- Description: The risk of developing kidney disease increases with age. Older adults often experience a natural decline in kidney function.
- Statistics: CKD is more prevalent in individuals over 60 years old.
- Family History:
- Description: A family history of kidney disease increases an individual’s risk, particularly for genetic conditions like PKD.
- Genetics: Certain hereditary syndromes predispose individuals to kidney disorders.
- Obesity:
- Description: Excess body weight can lead to conditions such as diabetes and hypertension, increasing the risk of kidney disease.
- Mechanism: Obesity contributes to metabolic syndrome, which is linked to kidney damage.
- Smoking:
- Description: Tobacco use has been associated with an increased risk of CKD and worsened kidney function.
- Mechanism: Smoking can reduce blood flow to the kidneys and promote hypertension.
- Chronic Diseases:
- Description: Conditions like diabetes and hypertension are significant risk factors for CKD.
- Management: Effective management of these conditions is crucial for kidney health.
- Ethnicity and Race:
- Description: Certain populations, such as African Americans, Hispanic Americans, and Native Americans, are at higher risk for kidney disease.
- Contributing Factors: Genetic predisposition, socioeconomic factors, and access to healthcare may play roles.
- Low Socioeconomic Status:
- Description: Individuals from lower socioeconomic backgrounds may have limited access to healthcare, leading to undiagnosed or poorly managed conditions.
- Consequences: Higher rates of diabetes and hypertension in these populations contribute to increased kidney disease risk.
- High Protein Diet:
- Description: Diets high in protein can increase the kidneys’ workload, potentially leading to damage over time, especially in individuals with preexisting conditions.
- Balance: Moderation and proper dietary planning are essential.
- Dehydration:
- Description: Chronic dehydration can lead to kidney damage, particularly in individuals prone to kidney stones or urinary tract issues.
- Prevention: Staying well-hydrated is crucial for kidney health.
Understanding the causes and risk factors of kidney disease is essential for prevention, early detection, and effective management. Regular check-ups, monitoring risk factors, and adopting a healthy lifestyle can significantly reduce the risk of developing kidney disease. Individuals with risk factors should consult healthcare professionals for personalized advice and interventions.
Symptoms of Kidney Disease
1. Early Symptoms
In the early stages of kidney disease, symptoms may be mild or absent. However, as the disease progresses, individuals may begin to notice various signs:
- Fatigue: A common symptom due to the accumulation of toxins in the body and reduced red blood cell production.
- Changes in Urination:
- Increased Frequency: Needing to urinate more often, especially at night (nocturia).
- Decreased Urine Output: Producing less urine than usual.
- Foamy or Bubbly Urine: Indicates the presence of protein, a sign of kidney damage.
- Blood in Urine (Hematuria): Can appear as pink, red, or cola-colored urine, indicating potential kidney injury or disease.
2. Fluid Retention Symptoms
As kidney function declines, the body may retain excess fluid, leading to:
- Swelling (Edema): Noticeable swelling in the legs, ankles, feet, or around the eyes.
- Shortness of Breath: Fluid accumulation in the lungs can cause difficulty breathing, especially during physical activity or when lying down.
3. Electrolyte Imbalance Symptoms
Kidneys help regulate electrolyte levels. An imbalance can lead to:
- Muscle Cramps: Caused by low levels of calcium and magnesium.
- Nausea and Vomiting: Accumulation of waste products and toxins can lead to gastrointestinal distress.
- Loss of Appetite: A decreased desire to eat due to nausea or the body’s inability to process nutrients effectively.
4. Systemic Symptoms
Kidney disease can have widespread effects on the body, leading to:
- High Blood Pressure: The kidneys play a crucial role in regulating blood pressure, and kidney dysfunction can lead to hypertension.
- Itching (Pruritus): Buildup of waste products can cause skin irritation and itching.
- Dry Skin: Changes in skin condition due to reduced kidney function.
5. Anemia-Related Symptoms
Reduced production of erythropoietin (a hormone produced by the kidneys) can lead to anemia, resulting in:
- Paleness: Noticeable pale skin due to reduced red blood cells.
- Weakness and Fatigue: Generalized weakness and lack of energy due to insufficient oxygen delivery to tissues.
6. Late-Stage Symptoms
In advanced stages of kidney disease (end-stage renal disease), symptoms become more severe:
- Severe Fatigue: Constant tiredness that interferes with daily activities.
- Confusion or Difficulty Concentrating: Accumulation of toxins can affect cognitive function.
- Seizures: In extreme cases, electrolyte imbalances can lead to seizures.
- Coma: Advanced kidney failure can result in loss of consciousness or coma due to severe toxicity.
Recognizing the symptoms of kidney disease is vital for early detection and intervention. Many symptoms can be subtle or mistaken for other conditions, so regular check-ups and monitoring are essential, especially for individuals at higher risk. If you or someone you know experiences any of these symptoms, it’s important to consult a healthcare professional for evaluation and appropriate management. Early intervention can significantly slow the progression of kidney disease and improve outcomes.
Diagnosis of Kidney Disease
Diagnosing kidney disease involves a combination of medical history, physical examination, laboratory tests, and imaging studies. Here’s a detailed breakdown:
1. Medical History and Physical Examination
- Medical History:
- The healthcare provider will inquire about symptoms, family history of kidney disease, personal medical history (e.g., diabetes, hypertension), and lifestyle factors (e.g., smoking, diet).
- Questions may also focus on any medications currently being taken, as some can affect kidney function.
- Physical Examination:
- A physical exam may include checking for signs of fluid retention (swelling in the legs or around the eyes) and assessing blood pressure.
2. Laboratory Tests
a. Blood Tests:
- Serum Creatinine: Measures the level of creatinine, a waste product produced by muscle metabolism. Elevated levels indicate reduced kidney function.
- Blood Urea Nitrogen (BUN): Assesses the concentration of urea in the blood. Elevated BUN can signal kidney dysfunction.
- Glomerular Filtration Rate (GFR): Estimated from serum creatinine levels to assess how well the kidneys are filtering blood. A GFR below 60 mL/min indicates possible kidney disease, while a GFR below 15 mL/min suggests kidney failure.
b. Urine Tests:
- Urinalysis: A comprehensive test that examines the appearance, concentration, and content of urine. It can detect abnormalities such as protein, blood, glucose, or signs of infection.
- 24-Hour Urine Collection: Measures the total volume of urine and assesses levels of specific substances, such as protein, electrolytes, and creatinine, providing a more comprehensive view of kidney function.
3. Imaging Studies
a. Ultrasound:
- Description: A non-invasive imaging technique that uses sound waves to create images of the kidneys. It can help identify structural abnormalities, kidney size, cysts, stones, or obstructions.
- Usefulness: It’s often the first imaging test performed when kidney disease is suspected.
b. CT Scan (Computed Tomography):
- Description: Provides detailed cross-sectional images of the kidneys and surrounding structures.
- Usefulness: Useful for detecting kidney stones, tumors, and other abnormalities that may not be visible on ultrasound.
c. MRI (Magnetic Resonance Imaging):
- Description: Uses magnetic fields and radio waves to create detailed images of the kidneys.
- Usefulness: Helpful for assessing kidney structure and blood vessels, especially in complex cases.
4. Kidney Biopsy
- Description: Involves removing a small sample of kidney tissue for laboratory analysis.
- Indications: Used when specific kidney disease is suspected (e.g., glomerulonephritis) or when the cause of kidney dysfunction is unclear.
- Procedure: Typically performed under local anesthesia using ultrasound or CT guidance to ensure accurate placement of the biopsy needle.
- Analysis: The tissue sample is examined microscopically for signs of inflammation, scarring, or other abnormalities.
5. Additional Tests
- Electrolyte Levels: Blood tests to measure levels of key electrolytes (e.g., potassium, sodium, calcium) can indicate kidney function and help guide treatment.
- Anemia Testing: Hemoglobin levels may be tested to check for anemia, common in chronic kidney disease due to reduced erythropoietin production.
Diagnosing kidney disease requires a thorough approach combining clinical evaluation and various tests. Early diagnosis is critical for effective management and can help slow the progression of kidney disease. If you experience symptoms or have risk factors for kidney disease, consult a healthcare professional for appropriate evaluation and testing. Regular monitoring is especially important for individuals with chronic conditions such as diabetes or hypertension.
Treatment and Management of Kidney disease
1. Lifestyle Modifications
a. Diet:
- Kidney-Friendly Diet: A balanced diet is crucial for managing kidney disease. Recommendations may include:
- Low Sodium: Reducing salt intake helps control blood pressure and reduces fluid retention.
- Protein Management: Depending on the stage of kidney disease, protein intake may need to be limited to reduce the kidneys’ workload.
- Fluid Intake: Monitoring fluid intake can help prevent overload, especially in advanced stages.
- Limit Potassium and Phosphorus: Foods high in potassium (e.g., bananas, oranges) and phosphorus (e.g., dairy, nuts) may need to be limited to prevent complications.
b. Physical Activity:
- Regular exercise helps maintain a healthy weight, control blood pressure, and improve overall health. Activities should be tailored to the individual’s abilities and health status.
c. Weight Management:
- Achieving and maintaining a healthy weight can reduce the risk of further kidney damage and improve overall health.
d. Smoking Cessation:
- Quitting smoking is essential, as it can worsen kidney disease and increase the risk of cardiovascular complications.
e. Alcohol Moderation:
- Limiting alcohol consumption is advisable, as excessive alcohol can adversely affect kidney function and overall health.
2. Medications
a. Control of Underlying Conditions:
- Antihypertensives: Medications like ACE inhibitors or angiotensin II receptor blockers (ARBs) help control blood pressure and have protective effects on the kidneys.
- Diabetes Management: Medications (e.g., metformin, insulin) are essential for controlling blood sugar levels in diabetic patients to prevent further kidney damage.
b. Anemia Management:
- Erythropoiesis-Stimulating Agents (ESAs): Medications like epoetin alfa can help stimulate red blood cell production in individuals with anemia due to chronic kidney disease.
- Iron Supplements: If iron deficiency is present, iron supplements may be prescribed.
c. Phosphate Binders:
- Used to control phosphate levels in the blood, helping prevent bone disease and other complications.
d. Diuretics:
- May be prescribed to help manage fluid retention and high blood pressure.
3. Dialysis
For individuals with end-stage renal disease (ESRD) or severe kidney dysfunction, dialysis may be necessary to perform the kidneys’ filtering functions:
a. Hemodialysis:
- Description: Blood is filtered through a machine to remove waste products and excess fluids.
- Frequency: Typically performed three times a week in a dialysis center or at home.
- Process: Access to the bloodstream is established through a fistula, graft, or catheter.
b. Peritoneal Dialysis:
- Description: Uses the lining of the abdomen (peritoneum) as a filter to remove waste products.
- Types: Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD).
- Home-Based: This method can often be done at home, providing more flexibility for patients.
4. Kidney Transplantation
When kidneys fail completely, a kidney transplant may be the best option:
- Criteria for Transplant: Candidates are assessed based on overall health, age, and kidney function. Transplants may come from living donors or deceased donors.
- Benefits: A successful transplant can restore normal kidney function and improve quality of life.
- Post-Transplant Care: Requires lifelong immunosuppressive medications to prevent rejection of the new kidney and regular monitoring of kidney function.
5. Regular Monitoring and Follow-Up
- Routine Check-Ups: Regular visits to healthcare providers are essential for monitoring kidney function, blood pressure, and overall health.
- Lab Tests: Periodic blood tests to assess serum creatinine, GFR, electrolyte levels, and anemia status.
- Adjustment of Treatment: Treatment plans may need to be adjusted based on changes in kidney function, symptoms, and lab results.
Effective management of kidney disease involves a comprehensive approach that includes lifestyle modifications, medications, and, in some cases, dialysis or transplantation. Early detection and intervention are critical in slowing disease progression and improving outcomes. Patients should work closely with healthcare providers to create a personalized management plan that addresses their specific needs and conditions. Regular monitoring and proactive management can significantly enhance quality of life and reduce complications associated with kidney disease.

Kidney disease is a serious condition that requires early detection and management to prevent complications and preserve kidney function. Understanding the types, causes, symptoms, and treatment options is essential for individuals at risk or those diagnosed with kidney disease. Lifestyle changes, medications, and regular medical follow-ups are crucial for effective management. If you suspect kidney problems or have risk factors, consult a healthcare professional for evaluation and guidance.