Psoriasis is a chronic autoimmune condition that primarily affects the skin, leading to the rapid buildup of skin cells. This results in scaling on the skin’s surface, which can cause discomfort, itching, and inflammation. While psoriasis is often recognized for its visible symptoms, it can also have systemic effects and is linked to other health conditions.
Types of Psoriasis
- Plaque Psoriasis:
- Description: The most common form, characterized by raised, red patches covered with thick, silvery scales. These plaques typically appear on elbows, knees, scalp, and lower back.
- Symptoms: Dry, cracked skin that may bleed, itching, and soreness.
- Guttate Psoriasis:
- Description: Often starts in childhood or young adulthood. It appears as small, drop-shaped lesions and is commonly triggered by bacterial infections, such as strep throat.
- Symptoms: Small, red spots on the torso, arms, legs, and scalp.
- Inverse Psoriasis:
- Description: Occurs in skin folds, such as under the breasts, in the groin, and around the buttocks. It presents as smooth, red patches without the typical scaling.
- Symptoms: Inflammation and discomfort in areas where skin rubs together.
- Pustular Psoriasis:
- Description: Characterized by white pustules (blisters of non-infectious pus) surrounded by red skin. It can be localized (on hands and feet) or generalized.
- Symptoms: Pustules, itching, and red skin; may be associated with fever and chills in severe cases.
- Erythrodermic Psoriasis:
- Description: A severe and rare form affecting most of the body surface. It can be life-threatening and requires immediate medical attention.
- Symptoms: Intense redness, shedding of skin in sheets, severe itching, and pain.
- Nail Psoriasis:
- Description: Affects the nails, causing pitting, abnormal nail growth, and discoloration. It can lead to nail lifting from the nail bed.
- Symptoms: Thickened nails, pitting, and separation from the nail bed.
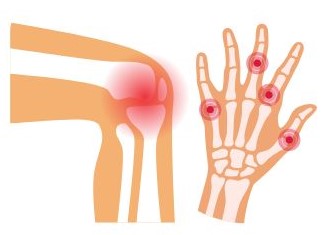
- Psoriatic Arthritis:
- Description: A type of inflammatory arthritis that affects some people with psoriasis. It can lead to joint pain, stiffness, and swelling.
- Symptoms: Joint pain, swelling, and changes in nails; may occur before or after skin symptoms.
Causes and Risk Factors
- Genetics:
- Psoriasis has a hereditary component, with a higher risk among those with a family history of the condition.
- Immune System:
- Psoriasis is an autoimmune disease, meaning the immune system mistakenly attacks healthy skin cells, leading to inflammation and rapid skin cell turnover.
- Environmental Triggers:
- Certain factors can trigger or exacerbate psoriasis symptoms, including:
- Infections: Such as strep throat or skin infections.
- Stress: Can worsen symptoms or trigger flare-ups.
- Skin Injuries: Cuts, scrapes, or severe sunburns can lead to new lesions (Koebner phenomenon).
- Weather: Cold, dry weather can worsen symptoms.
- Medications: Some drugs, like beta-blockers and lithium, may trigger or worsen psoriasis.
- Certain factors can trigger or exacerbate psoriasis symptoms, including:
- Lifestyle Factors:
- Obesity: Excess weight can increase the severity of psoriasis.
- Smoking: Linked to an increased risk of psoriasis and can worsen symptoms.
- Alcohol Consumption: Excessive drinking may trigger or exacerbate psoriasis flare-ups.
Symptoms of Psoriasis
Psoriasis can present a range of symptoms, and their severity can vary widely among individuals. Here’s a breakdown of the common symptoms associated with different types of psoriasis:
1. Plaque Psoriasis
- Appearance: Raised, red patches (plaques) covered with silvery-white scales. These plaques often have well-defined edges.
- Location: Commonly found on the elbows, knees, scalp, lower back, and sometimes the face.
- Associated Symptoms:
- Itching: Varies from mild to severe; can lead to scratching and potential skin damage.
- Soreness: Affected areas may feel tender or painful, especially if the skin is cracked.
2. Guttate Psoriasis
- Appearance: Small, drop-shaped lesions that are usually less than 1 cm in diameter.
- Location: Often appears on the trunk, arms, legs, and scalp.
- Associated Symptoms:
- Itching or discomfort: Can vary, but is often present.
- Triggers: Often associated with infections, especially streptococcal throat infections.
3. Inverse Psoriasis
- Appearance: Smooth, red patches without the typical scales, often shiny.
- Location: Found in skin folds such as under the breasts, in the groin, armpits, and around the buttocks.
- Associated Symptoms:
- Irritation and discomfort: May be exacerbated by friction and sweating.
- Itching: Often intense, leading to scratching.
4. Pustular Psoriasis
- Appearance: White pustules (blisters of non-infectious pus) surrounded by red skin.
- Location: Can be localized (often on the hands and feet) or generalized, affecting larger areas of the body.
- Associated Symptoms:
- Fever and chills: Especially in the generalized form, symptoms can include systemic reactions.
- Severe itching and burning: Pustules may be painful, and skin can be sensitive.
5. Erythrodermic Psoriasis
- Appearance: Widespread redness covering large areas of the body, sometimes appearing as a severe sunburn.
- Location: Affects most of the body surface.
- Associated Symptoms:
- Severe itching or burning: This form can be extremely uncomfortable.
- Systemic Symptoms: May include fever, chills, dehydration, and increased heart rate. This is a medical emergency and requires immediate attention.
6. Nail Psoriasis
- Appearance: Changes in the nails, including pitting, discoloration, and thickening. Nails may become brittle or separate from the nail bed.
- Location: Affects fingers and toes.
- Associated Symptoms:
- Nail Damage: Can lead to loss of the nail in severe cases.
- Discomfort: Pain may occur if nails are affected significantly.
7. Psoriatic Arthritis
- Appearance: Joint pain and swelling, which can be accompanied by skin lesions.
- Location: Can affect any joint, often in the fingers, toes, and spine.
- Associated Symptoms:
- Stiffness: Particularly in the morning or after periods of inactivity.
- Fatigue: General feeling of tiredness or malaise.
Additional Considerations
- Emotional Impact: Many individuals with psoriasis experience emotional symptoms such as anxiety, depression, or low self-esteem due to the visible nature of the skin condition and its potential impact on social interactions.
- Flare-Ups: Symptoms can be cyclical, with periods of flare-ups followed by remission. Triggers such as stress, infections, skin injuries, and changes in weather can provoke flare-ups.
- Comorbid Conditions: Patients with psoriasis are at higher risk for other health issues, including cardiovascular disease, metabolic syndrome, and depression, which can complicate symptom management.
The symptoms of psoriasis can vary greatly based on the type and severity of the condition. While the physical manifestations are often the most visible, the emotional and psychological impacts can be equally significant. Understanding the full range of symptoms can help individuals seek appropriate treatment and support. If you or someone you know is experiencing symptoms of psoriasis, it is essential to consult a healthcare professional for an accurate diagnosis and tailored management plan.
Diagnosis of Psoriasis
Diagnosing psoriasis typically involves a combination of clinical evaluation and, in some cases, laboratory tests. The following steps are commonly taken in the diagnostic process:
1. Medical History
- Patient Symptoms: The healthcare provider will begin by asking about the symptoms experienced, including their onset, duration, and severity. Important details include:
- Description of skin changes (e.g., scaling, redness).
- Areas of the body affected.
- Any associated symptoms like itching or pain.
- Family History: A family history of psoriasis or other autoimmune conditions can provide significant clues, as psoriasis often runs in families.
- Triggers: Patients may be asked about potential triggers, such as:
- Recent infections (e.g., strep throat).
- Stressful events or changes in lifestyle.
- Skin injuries or sunburn.
- Medications taken (some can exacerbate psoriasis).
2. Physical Examination
- Visual Inspection: A thorough physical examination is performed to assess the skin, scalp, and nails for typical psoriasis signs, including:
- Red, raised plaques with silvery scales.
- Locations of lesions (common areas include elbows, knees, scalp, and lower back).
- Nail changes (e.g., pitting, discoloration).
- Assessment of Severity: The provider may evaluate the extent of skin involvement, often using the Psoriasis Area and Severity Index (PASI), which scores the severity and extent of the disease.
3. Diagnostic Tests
While a diagnosis of psoriasis is primarily clinical, additional tests may be used in certain situations:
- Skin Biopsy:
- Purpose: A small sample of skin may be taken to confirm the diagnosis, particularly when the appearance is atypical or when other skin conditions (like eczema or dermatitis) are suspected.
- Analysis: The biopsy is examined under a microscope for characteristic changes, such as:
- Thickened epidermis (the outer skin layer).
- A high turnover of skin cells.
- Presence of inflammatory cells.
- Blood Tests:
- While there is no specific blood test for psoriasis, blood tests may be done to assess for other conditions or to evaluate overall health.
- Tests may include:
- Complete Blood Count (CBC): To check for signs of infection or anemia.
- Liver and Kidney Function Tests: Especially if systemic medications are being considered for treatment.
- Imaging Studies:
- If psoriatic arthritis is suspected, imaging tests like X-rays or MRIs may be used to assess joint health and detect any changes.
4. Differential Diagnosis
- Ruling Out Other Conditions: It’s important for healthcare providers to differentiate psoriasis from other skin conditions that may have similar symptoms, such as:
- Eczema: Typically characterized by itching and inflammation, often with a different distribution and appearance.
- Seborrheic Dermatitis: May cause scaly patches, particularly on the scalp, but typically lacks the thick plaques seen in psoriasis.
- Fungal Infections: Ringworm or other fungal skin infections can mimic some forms of psoriasis.
- Lichen Planus: An inflammatory condition that may present with similar lesions but usually has different characteristics.
5. Referral to a Specialist
- Dermatologist Consultation: In complex cases or when the diagnosis is uncertain, a referral to a dermatologist may be necessary for further evaluation and management.
Diagnosing psoriasis involves a thorough assessment of the patient’s history and symptoms, combined with a physical examination and, when necessary, diagnostic tests. Early and accurate diagnosis is crucial for effective management and treatment of the condition. If you suspect you have psoriasis or are experiencing symptoms, it’s important to consult a healthcare professional for evaluation and guidance tailored to your specific situation.
Treatment and Management
1. Topical Treatments
Topical therapies are often the first line of treatment for mild to moderate psoriasis. They are applied directly to the affected skin and can help reduce inflammation, scaling, and itching.
- Corticosteroids:
- Mechanism: Reduce inflammation and suppress the immune response.
- Forms: Available as creams, ointments, or lotions.
- Considerations: Potency varies; stronger formulations may be used for thicker plaques but should be used with caution to avoid side effects, such as skin thinning.
- Vitamin D Analogues:
- Examples: Calcipotriene and calcitriol.
- Mechanism: Slow down skin cell growth and reduce scaling.
- Use: Often combined with corticosteroids for enhanced effectiveness.
- Retinoids:
- Example: Tazarotene.
- Mechanism: A vitamin A derivative that helps normalize skin cell growth and reduces inflammation.
- Considerations: Can cause skin irritation; often used for plaque psoriasis.
- Calcineurin Inhibitors:
- Examples: Tacrolimus and pimecrolimus.
- Mechanism: Non-steroidal anti-inflammatory agents that reduce immune response in the skin.
- Use: Particularly useful for sensitive areas like the face and genitals.
- Salicylic Acid:
- Mechanism: Helps to remove scales and reduce inflammation.
- Form: Available in shampoos, creams, and ointments.
2. Phototherapy
Phototherapy involves exposing the skin to ultraviolet (UV) light under medical supervision and can be effective for moderate to severe psoriasis.
- UVB Phototherapy:
- Description: Uses broadband or narrowband UVB light.
- Frequency: Typically administered 2-3 times a week.
- Effectiveness: Can significantly improve symptoms and is often used for widespread psoriasis.
- PUVA (Psoralen + UVA):
- Description: Combines the use of a medication (psoralen) that sensitizes the skin to UVA light.
- Considerations: May be more effective for severe cases but requires careful monitoring due to potential side effects.
- Excimer Laser:
- Description: Targets specific areas of psoriasis with a focused beam of UVB light.
- Effectiveness: Effective for localized plaques and often requires fewer sessions.
3. Systemic Treatments
For moderate to severe psoriasis or when topical and phototherapy options are ineffective, systemic treatments may be necessary. These medications affect the entire body and can include:
- Oral Medications:
- Methotrexate: Suppresses the immune system and slows down cell growth. Often used for severe psoriasis and psoriatic arthritis.
- Cyclosporine: An immunosuppressant that can provide rapid relief but is typically used short-term due to side effects.
- Acitretin: A systemic retinoid that can help reduce skin cell production. Primarily used for severe cases and works best in combination with phototherapy.
- Biologics:
- Description: Target specific components of the immune system involved in psoriasis.
- Examples:
- TNF-alpha inhibitors (e.g., adalimumab, etanercept).
- IL-17 inhibitors (e.g., secukinumab).
- IL-12/23 inhibitors (e.g., ustekinumab).
- Administration: Typically administered by injection or infusion, and are used for moderate to severe psoriasis, especially when other treatments have failed.
- Benefits: Often result in significant and long-lasting improvement, but may increase the risk of infections and require regular monitoring.
4. Lifestyle Modifications
Integrating lifestyle changes can significantly improve psoriasis management and reduce flare-ups:
- Moisturization:
- Regularly applying emollients can help keep the skin hydrated and reduce dryness and scaling.
- Stress Management:
- Techniques such as yoga, meditation, and regular exercise can help manage stress, a common trigger for flare-ups.
- Healthy Diet:
- Maintaining a balanced diet rich in fruits, vegetables, whole grains, and healthy fats may help reduce inflammation. Omega-3 fatty acids, found in fish and flaxseed, are particularly beneficial.
- Avoiding Triggers:
- Identifying and avoiding personal triggers (e.g., smoking, alcohol, certain medications) can help prevent flare-ups.
5. Support and Education
- Patient Education: Understanding psoriasis and its triggers empowers individuals to take an active role in their treatment.
- Support Groups: Connecting with others who have psoriasis can provide emotional support and practical coping strategies.
- Counseling: Professional help can be beneficial for those struggling with the emotional impact of living with a chronic condition.
6. Regular Monitoring and Follow-Up
- Routine Check-Ups: Regular visits to a healthcare provider are essential for monitoring the condition, adjusting treatment plans, and managing any side effects from medications.
- Assessing Treatment Efficacy: Providers will evaluate the effectiveness of current treatments and make necessary adjustments based on the patient’s response and any emerging symptoms.
Managing psoriasis involves a multifaceted approach tailored to the individual’s needs and the severity of their condition. From topical treatments to systemic therapies, lifestyle modifications, and emotional support, a comprehensive strategy can significantly improve quality of life. Collaboration with healthcare providers is crucial for effective management and to ensure the best possible outcomes. If you or someone you know is struggling with psoriasis, seeking guidance from a healthcare professional can help in developing a personalized treatment plan.

Psoriasis is a complex, chronic autoimmune condition that requires a multifaceted approach for effective management. While there is currently no cure, many treatments can help control symptoms and improve quality of life. Early diagnosis and individualized treatment plans are essential for managing this condition. If you suspect you have psoriasis or are experiencing symptoms, consult a healthcare professional for evaluation and guidance.