Gout is a complex and often misunderstood form of arthritis that has been documented for centuries, earning it the nickname “the disease of kings.” This chronic condition is marked by sudden and severe episodes of joint pain, primarily caused by the accumulation of uric acid in the bloodstream, which can crystallize in the joints and surrounding tissues. While it is commonly associated with lifestyle factors and dietary choices, gout can also be influenced by genetic predispositions and underlying health conditions.
Gout typically presents itself in acute attacks, characterized by intense pain, swelling, and redness, most frequently affecting the big toe. However, it can impact other joints as well, such as the knees, ankles, and wrists. The pain can be debilitating, leading to significant discomfort and impacting daily activities.
Despite its historical connotations of excess and indulgence, gout is increasingly recognized as a prevalent and serious health issue affecting millions of people worldwide. Understanding gout is essential for effective management and prevention. With appropriate lifestyle changes, medical interventions, and awareness of triggers, individuals can reduce the frequency and severity of gout attacks, ultimately improving their quality of life.
In this article, we will delve into the causes and symptoms of gout, explore diagnosis and treatment options, and discuss preventive measures to help manage this condition effectively. Whether you are seeking to understand gout for yourself or to support someone else, this comprehensive overview aims to provide valuable insights into this complex disease.
1. What is Gout?
Overview:
Gout is a complex form of arthritis that occurs when uric acid, a waste product formed from the breakdown of purines (found in certain foods and drinks), accumulates in the body. Elevated uric acid levels can lead to the formation of sharp crystals in joints, causing intense inflammation and pain.
Types of Gout:
Gout can be classified into several types based on the nature and frequency of the attacks, as well as the underlying mechanisms involved. Understanding these types is essential for proper diagnosis and management. Here are the primary classifications of gout:
1. Acute Gout
Overview:
Acute gout is characterized by sudden and severe attacks of pain, often occurring at night or early morning. These episodes can last for hours to days and may resolve spontaneously or with treatment.
Symptoms:
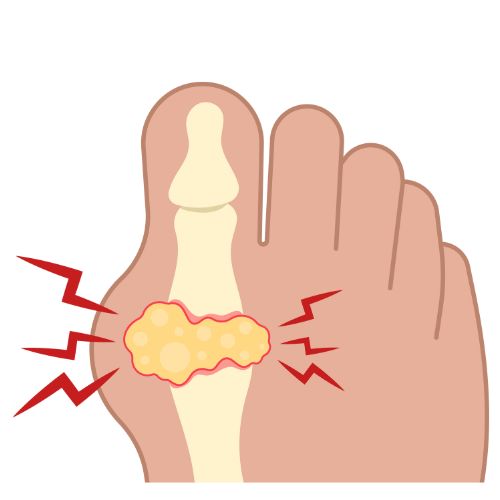
- Intense pain in the affected joint, typically the big toe (podagra).
- Swelling, redness, and warmth in the affected area.
- Increased sensitivity in the joint, making even light touch painful.
Causes:
Acute attacks are often triggered by factors such as dietary indiscretions (high purine foods), alcohol consumption, dehydration, stress, or illness.
Management:
Treatment typically includes nonsteroidal anti-inflammatory drugs (NSAIDs), colchicine, or corticosteroids to relieve pain and inflammation during an attack.
2. Chronic Gout
Overview:
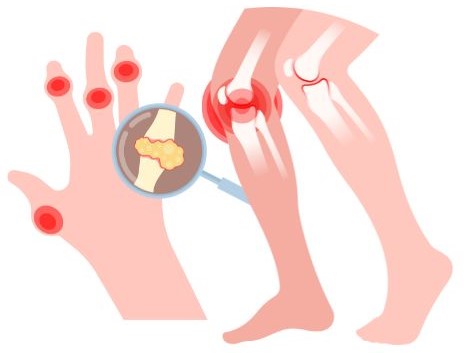
Chronic gout occurs when uric acid levels remain elevated over a prolonged period, leading to recurrent attacks and potential joint damage.
Symptoms:
- Frequent episodes of acute gout attacks, which can become more severe and longer-lasting over time.
- Persistent pain and discomfort in the joints, even between acute attacks.
- Development of tophi—hard, uric acid crystal deposits under the skin around joints.
Causes:
Chronic gout often results from untreated or poorly managed acute gout, along with ongoing factors like obesity, kidney disease, or certain medications that affect uric acid levels.
Management:
Long-term treatment typically involves urate-lowering therapy (ULT), such as allopurinol or febuxostat, along with lifestyle modifications to maintain healthy uric acid levels.
3. Pseudogout (Calcium Pyrophosphate Deposition Disease)
Overview:
While not a type of gout in the traditional sense, pseudogout mimics gout symptoms and is caused by the deposition of calcium pyrophosphate crystals in the joints instead of uric acid crystals.
Symptoms:
- Similar to gout, with sudden onset of joint pain, swelling, and redness, commonly affecting the knees.
- May occur without the classic triggers associated with gout attacks.
Causes:
Pseudogout is often associated with aging, certain metabolic conditions, and joint trauma.
Management:
Treatment may include NSAIDs, corticosteroids, or joint aspiration to relieve symptoms. Long-term management focuses on addressing any underlying conditions.
4. Intercritical Gout
Overview:
Intercritical gout refers to the periods between acute gout attacks when symptoms are not present but uric acid levels remain elevated.
Characteristics:
- Individuals may not experience any pain or inflammation during this phase, but they are still at risk for future attacks.
- Monitoring uric acid levels is essential to prevent transitions to chronic gout.
Management:
While there is no active treatment needed during these intervals, it is crucial to adopt lifestyle changes and possibly start urate-lowering medications to prevent future attacks.
Understanding the different types of gout is vital for effective management and treatment. While acute gout attacks are often the most recognizable, chronic gout and other related conditions like pseudogout can lead to more severe complications if not addressed. Proper diagnosis and individualized treatment plans, along with lifestyle modifications, can significantly improve outcomes and quality of life for those affected by gout. If you suspect you have gout or are experiencing symptoms, it’s important to consult a healthcare professional for guidance and support.
2. Causes of Gout
Gout is primarily caused by elevated levels of uric acid in the blood, a condition known as hyperuricemia. Several factors contribute to this increase in uric acid, which can lead to the formation of crystals in the joints and surrounding tissues. Here are the main causes and risk factors associated with gout:
1. Dietary Factors
Certain foods and beverages are high in purines, which the body breaks down into uric acid. Key dietary contributors include:
- Red Meat and Organ Meats: Foods such as beef, lamb, and liver contain high levels of purines.
- Seafood: Certain types of fish and shellfish, including sardines, anchovies, and scallops, can elevate uric acid levels.
- Alcohol: Beer and spirits can raise uric acid levels due to their purine content and can also impair the body’s ability to eliminate uric acid.
- Sugary Beverages: Drinks sweetened with high-fructose corn syrup, such as sodas and certain juices, are linked to higher uric acid levels.
2. Obesity
Excess body weight increases uric acid production and decreases its excretion through the kidneys. Fat tissue may also contribute to inflammation, exacerbating gout symptoms. Losing weight through diet and exercise can help lower uric acid levels and reduce the risk of gout attacks.
3. Genetics
Family history plays a significant role in an individual’s risk of developing gout. Certain genetic factors can affect how the body metabolizes purines and eliminates uric acid. If you have relatives with gout, your likelihood of developing the condition may be higher.
4. Medical Conditions
Several health conditions can contribute to the development of gout by affecting uric acid levels:
- Kidney Disease: Impaired kidney function can reduce the body’s ability to eliminate uric acid, leading to higher concentrations in the blood.
- Hypertension: High blood pressure is often associated with higher uric acid levels.
- Metabolic Syndrome: This cluster of conditions, which includes obesity, high blood pressure, and insulin resistance, is linked to an increased risk of gout.
- Diabetes and Insulin Resistance: These conditions can affect how the body processes and eliminates uric acid.
5. Medications
Certain medications can influence uric acid levels, either by increasing production or decreasing elimination. Common culprits include:
- Diuretics: Often prescribed for hypertension or heart conditions, diuretics can lead to higher uric acid levels by promoting fluid loss and concentrating uric acid in the bloodstream.
- Aspirin: Low-dose aspirin can interfere with uric acid excretion, potentially raising levels.
- Chemotherapy Drugs: Some cancer treatments can cause rapid cell turnover, releasing purines and increasing uric acid levels.
6. Dehydration
Inadequate fluid intake can lead to dehydration, which concentrates uric acid in the blood. Staying well-hydrated is important for maintaining proper kidney function and promoting the elimination of uric acid.
7. Age and Gender
Gout is more common in men than in women, particularly before menopause. This is partly due to hormonal differences that affect uric acid metabolism. As people age, the risk of developing gout increases due to cumulative exposure to risk factors and the decline in kidney function.
Gout is a multifactorial disease with various dietary, genetic, and health-related contributors to its development. Understanding the causes of gout is essential for effective prevention and management. By identifying and addressing these risk factors—such as dietary choices, weight management, and underlying health conditions—individuals can take proactive steps to reduce their risk of gout attacks and improve their overall health. If you suspect you are at risk or are experiencing symptoms, consulting a healthcare professional is crucial for guidance and support.
3. Symptoms of Gout
Gout typically presents itself in sudden and severe episodes, often referred to as gout attacks. Recognizing these symptoms early is crucial for effective management. Here’s a detailed overview of the symptoms associated with gout:
1. Acute Pain
- Sudden Onset: The hallmark of a gout attack is intense pain that can occur abruptly, often during the night or early morning.
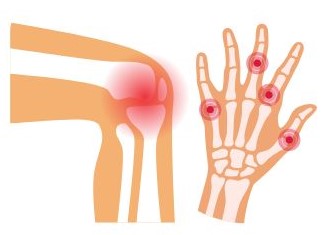
- Affected Joints: While the big toe (podagra) is the most common site, gout can also affect other joints, including the knees, ankles, elbows, wrists, and fingers.
- Pain Intensity: The pain is often described as throbbing, excruciating, or unbearable, making it difficult to walk or use the affected joint.
2. Swelling and Inflammation
- Joint Swelling: The affected joint usually becomes swollen and enlarged due to inflammation.
- Soft Tissue Swelling: Surrounding tissues may also swell, contributing to discomfort and limited movement.
3. Redness and Warmth
- Skin Changes: The skin over the affected joint may appear red, shiny, or warm to the touch, indicating inflammation.
- Color Variations: The redness can vary in intensity and may extend beyond the immediate area of the joint.
4. Limited Range of Motion
- Stiffness: As the attack progresses, stiffness in the affected joint may develop, leading to decreased range of motion.
- Difficulty Moving: Even gentle movements can cause significant pain, making daily activities challenging.
5. Duration of Symptoms
- Acute Attack Duration: An acute gout attack can last from a few hours to several days. Without treatment, the intensity of pain may peak within 12 to 24 hours and gradually decrease.
- Recurrence: Individuals may experience multiple attacks over time, with varying intervals between episodes.
6. Intercritical Periods
- Asymptomatic Phases: Between attacks, individuals may have no symptoms, but uric acid levels may remain elevated, putting them at risk for future attacks.
- Potential for Chronic Gout: Over time, repeated attacks can lead to chronic gout, where symptoms persist even between flare-ups.
7. Tophi Formation
- Chronic Condition Signs: In chronic gout, tophi may develop, which are visible lumps formed by the accumulation of uric acid crystals. They commonly appear around joints, in the ears, or on the fingers.
- Non-Painful: Tophi may not be painful but can indicate long-term uncontrolled uric acid levels and may lead to joint damage.
8. Systemic Symptoms
- Fever: Some individuals may experience mild fever during a gout attack.
- Malaise: General feelings of unwellness or fatigue can accompany acute attacks, adding to discomfort.
Recognizing the symptoms of gout is essential for early intervention and effective management. Acute pain, swelling, redness, and limited motion are characteristic signs of gout attacks, while tophi may indicate a chronic condition. If you experience these symptoms, particularly if they occur suddenly and are severe, it is important to consult a healthcare professional for accurate diagnosis and treatment. Early management can help prevent future attacks and reduce the risk of complications associated with chronic gout.
4. Diagnosis of Gout
Diagnosing gout involves a combination of medical history, physical examination, laboratory tests, and imaging studies. Accurate diagnosis is crucial for effective treatment and management. Here’s a detailed overview of the diagnostic process for gout:
1. Medical History
- Symptom Description: The healthcare provider will ask about the symptoms, including the onset, duration, and intensity of pain, swelling, and redness in the affected joints.
- Past Episodes: Information about previous gout attacks, their frequency, and how they were managed can provide important insights.
- Family History: A history of gout or other related conditions in the family may increase the likelihood of gout.
2. Physical Examination
- Joint Examination: A thorough examination of the affected joint(s) will be conducted to assess swelling, tenderness, warmth, and redness.
- Other Joints: The provider may also examine other joints to check for signs of tophi or previous joint damage.
3. Laboratory Tests
Several lab tests are commonly used to confirm a diagnosis of gout:
- Uric Acid Levels:
- Blood Test: A blood test measures the level of uric acid in the bloodstream. Elevated levels can indicate gout, but normal levels do not rule it out, as some individuals may still experience gout attacks with lower uric acid.
- Joint Fluid Analysis:
- Arthrocentesis: A needle is used to withdraw fluid from the affected joint. This synovial fluid is then analyzed under a microscope to check for the presence of uric acid crystals, which confirm a gout diagnosis.
- Complete Blood Count (CBC):
- This test may be performed to check for signs of inflammation or infection, such as elevated white blood cell counts.
4. Imaging Studies
Imaging can help assess joint damage and rule out other conditions:
- X-rays:
- While not definitive for diagnosing gout, X-rays can be used to rule out other causes of joint pain and to identify any joint damage or tophi that may have developed over time.
- Ultrasound:
- This imaging technique can visualize urate crystals in the joint fluid and detect tophi. It is a non-invasive method that can provide valuable information.
- Dual-Energy CT Scan:
- This advanced imaging technique can detect uric acid crystals in joints and soft tissues, even when other imaging methods may not show clear signs of gout.
5. Differential Diagnosis
Gout symptoms can mimic those of other conditions, so it’s essential to differentiate it from:
- Pseudogout: Caused by calcium pyrophosphate crystals rather than uric acid.
- Septic Arthritis: Joint infection that can present similarly but requires different management.
- Other Types of Arthritis: Conditions like rheumatoid arthritis or osteoarthritis may have overlapping symptoms.
A comprehensive approach combining medical history, physical examination, laboratory tests, and imaging studies is essential for accurately diagnosing gout. Early diagnosis and effective management can help alleviate symptoms, prevent future attacks, and reduce the risk of complications. If you suspect you have gout or are experiencing joint pain, it is important to consult a healthcare professional for proper evaluation and treatment.
5. Treatment Options for Gout
Managing gout involves both acute treatment to relieve symptoms during attacks and long-term strategies to lower uric acid levels and prevent future episodes. Here’s a detailed overview of the treatment options for gout:
1. Acute Gout Attack Management
When a gout attack occurs, the primary goal is to relieve pain and reduce inflammation. Common treatment options include:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
- Medications such as ibuprofen, naproxen, or indomethacin are often prescribed to alleviate pain and inflammation. These are typically taken at the onset of symptoms.
- Colchicine:
- Colchicine is effective in reducing pain, particularly if taken within the first 24 hours of an attack. It works by decreasing inflammation and can also prevent future attacks when taken regularly.
- Corticosteroids:
- Corticosteroids (e.g., prednisone) may be prescribed if NSAIDs or colchicine are ineffective or contraindicated. They can be administered orally or via injection directly into the affected joint for rapid relief.
- Rest and Ice:
- Resting the affected joint and applying ice can help reduce swelling and alleviate pain.
2. Long-Term Management
To prevent recurrent gout attacks and manage chronic gout, long-term treatment strategies are crucial:
- Urate-Lowering Therapy (ULT):
- Medications that lower uric acid levels are often prescribed for individuals with frequent attacks or chronic gout. Common ULT options include:
- Allopurinol: This medication reduces uric acid production and is commonly used for long-term management.
- Febuxostat: An alternative to allopurinol, it also lowers uric acid levels and may be preferred for those who cannot tolerate allopurinol.
- Probenecid: This medication helps the kidneys excrete more uric acid. It is less commonly used and may not be suitable for individuals with kidney problems.
- Medications that lower uric acid levels are often prescribed for individuals with frequent attacks or chronic gout. Common ULT options include:
- Lifestyle Modifications:
- Dietary Changes: Reducing the intake of purine-rich foods (red meat, seafood, alcohol, and sugary beverages) can help lower uric acid levels.
- Hydration: Drinking plenty of water helps the kidneys flush out uric acid more effectively.
- Weight Management: Losing weight can significantly reduce uric acid levels and the frequency of attacks. A gradual and sustainable weight loss approach is recommended.
- Regular Monitoring:
- Regular check-ups and blood tests to monitor uric acid levels are essential to assess the effectiveness of treatment and make adjustments as needed.
3. Managing Comorbidities
Since gout often coexists with other health conditions, managing these can also help reduce gout flares:
- Hypertension and Diabetes: Proper management of high blood pressure and diabetes can influence uric acid levels.
- Kidney Health: Maintaining kidney function is vital, as impaired kidney function can lead to higher uric acid levels.
4. Preventive Measures
In addition to medical treatments, preventive strategies are important:
- Avoiding Triggers: Identifying and avoiding personal triggers for gout attacks (such as specific foods or beverages) can help prevent future episodes.
- Medication Adherence: Consistently taking prescribed medications as directed is crucial for effective long-term management.
Effective treatment of gout requires a comprehensive approach that addresses both acute symptoms and long-term management strategies. By utilizing medications, lifestyle changes, and regular monitoring, individuals can significantly reduce the frequency and severity of gout attacks. If you experience symptoms of gout or have a history of gout attacks, consulting a healthcare professional for an individualized treatment plan is essential for maintaining optimal health and well-being.
6. Preventive Measures
Preventing gout attacks involves a combination of lifestyle modifications, dietary changes, and ongoing management strategies. Here’s a comprehensive look at effective preventive measures:
1. Dietary Changes
Making informed dietary choices is crucial for managing uric acid levels:
- Limit Purine-Rich Foods:
- Reduce consumption of foods high in purines, which break down into uric acid. These include:
- Red meats (beef, lamb, pork)
- Organ meats (liver, kidneys, sweetbreads)
- Certain seafood (anchovies, sardines, mussels, scallops)
- Reduce consumption of foods high in purines, which break down into uric acid. These include:
- Avoid Sugary Beverages:
- Limit intake of drinks sweetened with high-fructose corn syrup, such as sodas and some fruit juices, as these can elevate uric acid levels.
- Limit Alcohol:
- Alcohol, especially beer and spirits, can raise uric acid levels and trigger gout attacks. Moderation is key, and avoiding alcohol during high-risk periods is advisable.
- Incorporate Low-Fat Dairy:
- Low-fat dairy products may help lower uric acid levels and are a good source of protein. Consider including yogurt, milk, and cheese in your diet.
- Increase Fruit and Vegetable Intake:
- Aim for a diet rich in fruits, vegetables, and whole grains. Cherries, in particular, may help reduce the frequency of gout attacks due to their anti-inflammatory properties.
2. Hydration
- Stay Hydrated:
- Drinking plenty of water helps dilute uric acid in the blood and promotes its excretion through the kidneys. Aim for at least 8–10 glasses of water daily, or more if you are active or live in a hot climate.
3. Weight Management
- Achieve a Healthy Weight:
- Losing excess weight can significantly lower uric acid levels and reduce the risk of gout attacks. Aim for gradual weight loss through a balanced diet and regular exercise.
- Avoid Rapid Weight Loss:
- Rapid weight loss can temporarily increase uric acid levels, so it’s essential to adopt a steady and sustainable approach.
4. Regular Exercise
- Stay Active:
- Regular physical activity can help maintain a healthy weight, improve overall health, and reduce the risk of chronic conditions that may influence uric acid levels. Aim for at least 150 minutes of moderate exercise per week, incorporating both aerobic and strength-training activities.
5. Medication Adherence
- Consistent Use of Uric Acid-Lowering Medications:
- For individuals with a history of frequent gout attacks, adherence to prescribed medications such as allopurinol or febuxostat is essential for preventing future flares. Regular monitoring of uric acid levels may also be required.
6. Avoiding Known Triggers
- Identify Personal Triggers:
- Keep track of foods, drinks, or activities that precede gout attacks to help identify personal triggers. Avoiding these can help minimize the risk of future episodes.
7. Regular Health Check-ups
- Monitor Health Conditions:
- Regular visits to healthcare providers to monitor blood pressure, kidney function, and overall health can help manage conditions that may exacerbate gout.
- Blood Tests:
- Routine blood tests to monitor uric acid levels can guide treatment adjustments and help maintain levels within a safe range.
Preventing gout involves a proactive approach that combines dietary management, hydration, weight control, exercise, and medication adherence. By making these lifestyle changes and staying vigilant about potential triggers, individuals can significantly reduce the frequency and severity of gout attacks. If you have a history of gout or are at risk, consult a healthcare professional for personalized strategies and support to manage and prevent this condition effectively.

Gout is a painful and often debilitating condition that can significantly impact quality of life. Understanding the causes, recognizing the symptoms early, and seeking timely medical advice are crucial for effective management. With appropriate treatment and lifestyle modifications, individuals with gout can manage their condition and prevent future flare-ups. If you suspect you have gout or experience recurrent joint pain, consult a healthcare professional for proper diagnosis and treatment.