Osteoarthritis (OA) is the most common form of arthritis and a leading cause of disability worldwide. It is characterized by the degeneration of cartilage, the protective tissue at the ends of bones, leading to pain, stiffness, and impaired mobility. Understanding osteoarthritis, its symptoms, causes, diagnosis, and management options is essential for those affected and their caregivers.
What is Osteoarthritis?
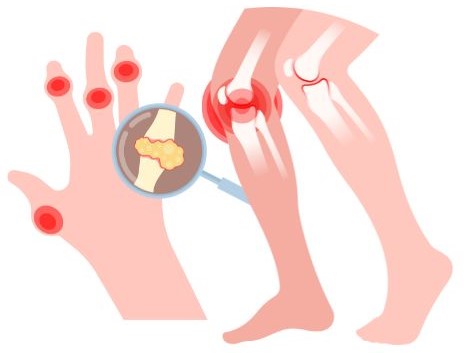
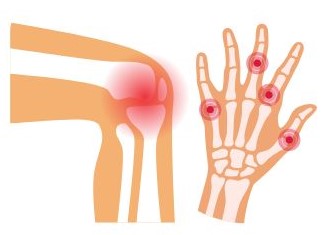
Osteoarthritis is a chronic condition that primarily affects the joints, including those in the hands, knees, hips, and spine. It occurs when cartilage breaks down, causing bones to rub against each other, which can result in pain and loss of joint function. OA can affect individuals of all ages but is more prevalent in older adults.
Key Features
- Cartilage Degeneration: The cushioning cartilage wears away, leading to increased friction between bones.
- Bone Changes: Osteophytes (bone spurs) may develop, and the underlying bone may thicken.
- Joint Inflammation: While inflammation is typically mild compared to other forms of arthritis, it can still occur.
Symptoms of Osteoarthritis
The symptoms of osteoarthritis can vary widely and may develop gradually over time. Common symptoms include:
- Joint Pain
- Pain is the hallmark symptom of osteoarthritis and can vary in intensity from mild to severe.
- Pain usually worsens with activity and improves with rest. It may be localized to specific joints, commonly affecting the knees, hips, hands, and spine.
- Stiffness
- Many individuals with osteoarthritis experience stiffness, particularly after periods of inactivity.
- Morning stiffness is common, typically lasting less than 30 minutes. Stiffness may also occur after sitting for long periods or after prolonged activity.
- Swelling
- Affected joints may become swollen due to inflammation or increased synovial fluid production.
- Swelling can lead to a feeling of warmth in the joint and may be accompanied by tenderness when pressure is applied.
- Decreased Range of Motion
- The ability to move the affected joint fully may be compromised.
- This limitation can hinder daily activities, such as bending down, climbing stairs, or gripping objects.
- Creaking or Cracking Sounds (Crepitus)
- A grating or cracking sensation may occur when moving the affected joint.
- This sound is due to the roughened surfaces of the joint rubbing against each other as the cartilage deteriorates.
- Tenderness
- Joints may feel tender to the touch.
- Tenderness is often experienced when pressure is applied to the affected area, making certain movements painful.
- Bone Spurs
- These are small bony growths that may develop around the affected joint.
- Bone spurs can contribute to joint pain and may further restrict movement.
- Joint Deformity
- In advanced stages of osteoarthritis, changes in bone structure can lead to visible deformities.
- Joints may appear enlarged or misshapen, particularly in the hands (e.g., Heberden’s nodes on the fingers).
- Fatigue
- Chronic pain and discomfort can lead to fatigue.
- Individuals may feel more tired due to the constant effort of managing pain and limitations in mobility.
- Psychological Symptoms
- The chronic nature of osteoarthritis can impact mental health.
- Individuals may experience feelings of frustration, anxiety, or depression as a result of living with chronic pain and functional limitations.
Progression of Symptoms
- Early Stages: Symptoms may start as mild discomfort or pain after activity, often mistaken for normal wear and tear.
- Moderate Stages: Pain and stiffness become more pronounced, occurring during and after activities, and joint swelling may be evident.
- Advanced Stages: Pain may become constant, even at rest, with significant joint damage and deformity. Daily activities may be severely impacted.
Recognizing and understanding the symptoms of osteoarthritis is essential for early diagnosis and effective management. If you or someone you know is experiencing these symptoms, it’s important to consult a healthcare provider for a comprehensive evaluation and to discuss potential treatment options. Early intervention can significantly improve quality of life and help manage the progression of the disease.
Causes and Risk Factors of Osteoarthritis
Causes:
- Cartilage Degeneration
- Description: Osteoarthritis is primarily caused by the gradual breakdown of cartilage, the smooth tissue that cushions the ends of bones in joints.
- Mechanism: As cartilage deteriorates, bones begin to rub against each other, leading to pain, swelling, and decreased mobility.
- Joint Injury
- Description: Previous injuries to a joint, such as fractures, dislocations, or ligament tears, can increase the likelihood of developing OA.
- Mechanism: These injuries can damage cartilage and the surrounding tissues, leading to inflammation and eventual degeneration.
- Overuse of Joints
- Description: Repetitive stress on joints from certain occupations or activities can contribute to the wear and tear of cartilage.
- Mechanism: Jobs that require heavy lifting, kneeling, or repetitive motions can accelerate the breakdown of cartilage, increasing the risk of OA.
- Genetic Factors
- Description: There is evidence suggesting that genetic predisposition plays a role in the development of osteoarthritis.
- Mechanism: Specific genes may affect cartilage structure and function, making certain individuals more susceptible to OA.
- Metabolic Factors
- Description: Conditions such as diabetes and obesity can impact joint health and contribute to the development of OA.
- Mechanism: Excess body weight increases stress on weight-bearing joints and can lead to inflammation, which exacerbates cartilage degradation.
Risk Factors:
- Age
- Description: The risk of developing osteoarthritis increases significantly with age.
- Impact: Natural wear and tear on joints over time can lead to cartilage deterioration, making older adults more susceptible.
- Obesity
- Description: Excess weight puts additional stress on weight-bearing joints, such as the knees and hips.
- Impact: Obesity is a major modifiable risk factor for OA, as it not only increases mechanical load but also contributes to systemic inflammation.
- Gender
- Description: Women are more likely to develop osteoarthritis than men, particularly after menopause.
- Impact: Hormonal changes may influence joint health, and the prevalence of OA increases in postmenopausal women.
- Family History
- Description: A family history of osteoarthritis can increase an individual’s risk.
- Impact: Genetic factors may play a role in cartilage structure and susceptibility to joint degeneration.
- Joint Injuries
- Description: Previous injuries, such as fractures or ligament tears, can predispose individuals to OA in the affected joints.
- Impact: The severity of the injury and the age at which it occurs can influence the likelihood of developing osteoarthritis later in life.
- Repetitive Stress and Overuse
- Description: Engaging in repetitive activities or jobs that place strain on certain joints increases the risk of OA.
- Impact: Professions that involve heavy lifting, kneeling, or squatting can lead to accelerated joint wear.
- Other Health Conditions
- Description: Conditions like rheumatoid arthritis, metabolic disorders, and hormonal imbalances can contribute to joint health issues.
- Impact: Inflammatory diseases can increase the likelihood of developing osteoarthritis in affected joints.
- Sedentary Lifestyle
- Description: Lack of physical activity can lead to weakened muscles and reduced joint flexibility.
- Impact: Regular exercise helps maintain joint function and supports overall joint health, while inactivity can increase the risk of OA.
Osteoarthritis is influenced by a complex interplay of genetic, metabolic, and environmental factors. Understanding the causes and risk factors can aid in early detection, prevention, and effective management strategies. If you are concerned about your risk of osteoarthritis, consider discussing it with a healthcare provider for personalized advice and recommendations.
Diagnosis of Osteoarthritis
Diagnosing osteoarthritis typically involves a combination of the following:
1. Medical History
- Symptom Assessment: A detailed history of symptoms, including pain location, severity, and duration, is essential.
- Activity Level: Understanding how the condition affects daily activities helps in assessing its impact.
2. Physical Examination
- Joint Examination: A healthcare provider will examine affected joints for swelling, tenderness, range of motion, and any deformities.
3. Imaging Tests
- X-rays: These can reveal joint space narrowing, bone spurs, and other changes associated with OA.
- MRI: In some cases, MRI may be used to assess cartilage loss and other soft tissue changes.
4. Laboratory Tests
- While there are no specific blood tests for OA, tests may be conducted to rule out other types of arthritis or conditions that cause similar symptoms.
Management and Treatment
While there is no cure for osteoarthritis, various treatments can help manage symptoms and improve quality of life. Treatment plans are often individualized based on the severity of symptoms and the specific joints affected.
1. Lifestyle Modifications
- Weight Management: Maintaining a healthy weight can significantly reduce stress on weight-bearing joints, alleviating pain.
- Physical Activity: Engaging in low-impact exercises, such as swimming, walking, or cycling, can improve joint function and reduce stiffness. Physical therapy may also be beneficial.
2. Medications
- Analgesics: Over-the-counter pain relievers, such as acetaminophen, can help manage mild to moderate pain.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These include ibuprofen and naproxen and can help reduce pain and inflammation.
- Topical Treatments: Creams or gels containing NSAIDs or capsaicin can provide localized pain relief.
3. Physical Therapy
- Therapeutic Exercises: A physical therapist can develop a personalized exercise program to strengthen muscles around the affected joints and improve flexibility.
- Manual Therapy: Techniques such as massage and mobilization may help alleviate pain and improve function.
4. Injections
- Corticosteroid Injections: These can provide temporary relief from inflammation and pain in the affected joints.
- Hyaluronic Acid Injections: These may help lubricate the joint and reduce pain, particularly in the knee.
5. Assistive Devices
- Braces and Supports: These can help stabilize joints and alleviate stress during activities.
- Mobility Aids: Canes or walkers may assist in maintaining mobility and reducing pain.
6. Surgical Options
- Arthroscopy: A minimally invasive procedure to remove damaged tissue or debris from the joint.
- Joint Replacement Surgery: In severe cases, total or partial joint replacement may be considered, particularly for hips and knees.
Living with Osteoarthritis
1. Understanding Your Condition
- Education: Knowledge about osteoarthritis, including its causes, symptoms, and progression, empowers individuals to take charge of their health.
- Monitoring Symptoms: Keeping a journal of symptoms, activities, and triggers can help identify patterns and manage flare-ups more effectively.
2. Symptom Management
- Pain Relief Strategies:
- Over-the-Counter Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can help alleviate pain and reduce inflammation.
- Topical Treatments: Creams or gels containing NSAIDs or capsaicin can provide localized relief.
- Physical Therapy:
- Customized Exercise Plans: A physical therapist can design a program tailored to your needs, focusing on strengthening muscles around the joints, improving flexibility, and enhancing overall mobility.
- Manual Therapy: Techniques such as massage or mobilization can help alleviate pain and improve function.
3. Lifestyle Modifications
- Regular Exercise:
- Low-Impact Activities: Engage in activities like walking, swimming, or cycling, which are easier on the joints while still promoting fitness.
- Strength Training: Building muscle strength around affected joints can provide better support and reduce pain.
- Weight Management:
- Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help maintain a healthy weight.
- Caloric Awareness: Understanding caloric intake can assist in weight loss or maintenance, reducing stress on weight-bearing joints.
4. Assistive Devices
- Braces and Supports: Joint braces or sleeves can provide stability and support, particularly for knees and wrists.
- Mobility Aids: Canes, walkers, or other assistive devices can help maintain independence while reducing strain on joints.
5. Home Modifications
- Creating an Accessible Environment:
- Ergonomic Tools: Use tools that reduce strain, such as jar openers, reachers, or adaptive kitchen utensils.
- Bathroom Safety: Install grab bars and use non-slip mats to prevent falls.
- Temperature Therapy:
- Heat Therapy: Applying heat pads or taking warm baths can help relax muscles and alleviate stiffness.
- Cold Therapy: Using ice packs can reduce inflammation and numb pain during flare-ups.
6. Mental and Emotional Well-Being
- Managing Stress: Chronic pain can lead to increased stress and anxiety. Techniques such as meditation, yoga, or deep-breathing exercises can be beneficial.
- Counseling and Support Groups: Sharing experiences with others who understand can provide emotional support and practical coping strategies.
7. Regular Medical Check-Ups
- Routine Visits: Regular consultations with healthcare providers help monitor the progression of OA and adjust treatment plans as necessary.
- Alternative Therapies: Explore options like acupuncture, chiropractic care, or nutritional supplements (e.g., glucosamine) after discussing them with your doctor.
8. Creating a Support Network
- Family and Friends: Educating loved ones about OA can foster understanding and support. Involving them in activities or discussing challenges can improve emotional well-being.
- Support Groups: Joining a support group, either in-person or online, can connect you with others facing similar challenges, providing a sense of community.
9. Setting Realistic Goals
- Personalized Action Plan: Work with healthcare professionals to set achievable goals related to physical activity, weight loss, or symptom management.
- Celebrate Progress: Acknowledge small victories and milestones in your journey to manage OA effectively.
Living with osteoarthritis involves a proactive approach to managing symptoms and enhancing quality of life. By understanding the condition, implementing lifestyle changes, and seeking support, individuals can navigate the challenges of OA and maintain an active, fulfilling life. If you’re struggling with the impact of osteoarthritis, remember that a comprehensive management plan tailored to your needs can significantly improve your daily experience.

Osteoarthritis is a chronic condition that requires ongoing management and adaptation. By understanding the disease and employing effective treatment strategies, individuals can maintain a good quality of life and continue to engage in daily activities. If you or someone you know is experiencing symptoms of osteoarthritis, seeking medical advice is essential for an accurate diagnosis and appropriate management.