Rheumatoid arthritis (RA) is a chronic inflammatory disorder that primarily affects joints but can also impact other systems in the body. Understanding the symptoms, causes, and available treatments is crucial for managing this condition effectively.
What is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is a chronic autoimmune disorder characterized by inflammation of the joints and surrounding tissues. Unlike osteoarthritis, which is primarily a degenerative condition resulting from wear and tear, RA involves the immune system mistakenly attacking the synovium, the lining of the membranes that encapsulate joints. This autoimmune response leads to the production of inflammatory chemicals, resulting in pain, swelling, and eventually joint damage.
Key Features of Rheumatoid Arthritis
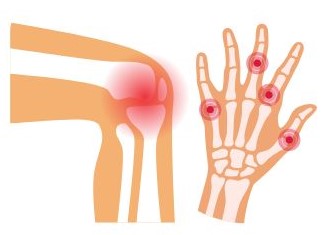
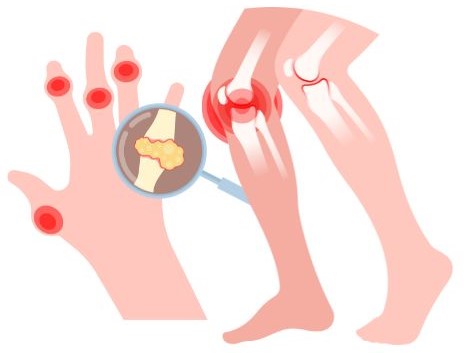
- Symmetrical Joint Involvement: RA typically affects joints on both sides of the body symmetrically. For example, if one knee is affected, the other knee is likely to be affected as well.
- Chronic Condition: RA is a lifelong condition with periods of flare-ups and remission. During flare-ups, symptoms can intensify, while during remission, symptoms may decrease or disappear entirely.
- Joint Damage: Over time, persistent inflammation can erode cartilage and bone, leading to deformities and loss of joint function. Early intervention is crucial to prevent irreversible damage.
- Extra-Articular Manifestations: RA can also affect other organs and systems, leading to complications such as:
- Cardiovascular issues: Increased risk of heart disease and inflammation of blood vessels.
- Lung problems: Interstitial lung disease and pleuritis.
- Ocular issues: Sjögren’s syndrome can cause dry eyes and mouth.
- Rheumatoid nodules: These are firm lumps that can form under the skin near joints, often in areas subject to pressure.
Symptoms of Rheumatoid Arthritis
The symptoms of rheumatoid arthritis (RA) can vary significantly from person to person, and they may change over time. Understanding these symptoms is vital for early diagnosis and effective management. Here’s a detailed look at the common and less common symptoms associated with RA:
Common Symptoms
- Joint Pain and Swelling:
- Location: RA typically affects smaller joints first, such as those in the hands and feet, but can also involve larger joints like the knees and shoulders.
- Nature: The pain is often symmetrical, meaning if one joint is affected, the corresponding joint on the other side of the body is likely to be affected as well.
- Morning Stiffness:
- Duration: Many individuals experience stiffness upon waking, lasting more than 30 minutes. This stiffness can also occur after sitting or resting for extended periods.
- Impact: Stiffness can make it difficult to perform daily activities, such as dressing or typing.
- Fatigue:
- Chronic Fatigue: Many people with RA report persistent tiredness that doesn’t improve with rest, which can significantly impact daily life and productivity.
- Fever:
- Low-Grade Fever: Some individuals may experience mild fevers during flare-ups, reflecting the underlying inflammation in the body.
- Weight Loss:
- Unintentional Weight Loss: Some individuals may lose weight due to decreased appetite or the body’s increased metabolic demands associated with inflammation.
- Nodules:
- Rheumatoid Nodules: These are firm lumps that can develop under the skin, typically near affected joints. They are often painless but can be uncomfortable, especially if they press on nerves.
Systemic Symptoms
RA is not limited to the joints; it can also have systemic effects on the body. Common systemic symptoms include:
- Anemia:
- Many individuals with RA develop anemia, a condition characterized by a decrease in red blood cells, which can lead to fatigue and weakness.
- Dry Eyes and Mouth:
- Sjögren’s Syndrome: RA can be associated with Sjögren’s syndrome, an autoimmune disorder that leads to dry eyes and dry mouth due to the immune system attacking the glands that produce moisture.
- Lung Complications:
- RA can cause inflammation of the lung tissue or pleura (lining of the lungs), leading to symptoms such as shortness of breath, cough, and chest pain.
- Cardiovascular Issues:
- People with RA are at an increased risk of developing heart disease and other cardiovascular problems due to chronic inflammation.
Less Common Symptoms
- Skin Changes:
- Some individuals may experience skin rashes or changes, including vasculitis (inflammation of blood vessels), which can lead to skin ulcers or other skin lesions.
- Nerve Damage:
- Compression of nerves in affected joints can lead to symptoms like tingling, numbness, or weakness in the extremities.
- Joint Deformities:
- Over time, persistent inflammation can cause deformities in the joints, such as swan-neck or boutonnière deformities in the fingers.
Flare-Ups and Remissions
RA symptoms can fluctuate, with periods of increased activity known as flare-ups, followed by periods of remission where symptoms decrease or disappear. The triggers for these flare-ups can vary and may include:
- Stress
- Illness or infection
- Changes in weather
- Physical overexertion
Recognizing the diverse symptoms of rheumatoid arthritis is crucial for early diagnosis and treatment. If you experience persistent joint pain, stiffness, or any of the systemic symptoms mentioned, it’s important to consult a healthcare professional. Early intervention can help manage symptoms effectively, reduce the risk of joint damage, and improve overall quality of life.
Causes of Rheumatoid Arthritis
The exact cause of rheumatoid arthritis (RA) remains unclear, but it is believed to result from a combination of genetic, environmental, and immunological factors. Understanding these potential causes can help in identifying risk factors and the mechanisms underlying the disease.
1. Genetic Factors
- Family History: Individuals with a family history of RA are at a higher risk, suggesting a genetic predisposition. Certain genes have been associated with an increased risk of developing the condition.
- HLA-DRB1 Gene: This gene, part of the human leukocyte antigen (HLA) complex, plays a critical role in the immune system. Variants of this gene have been strongly linked to an increased risk of RA.
2. Environmental Triggers
Certain environmental factors may trigger the onset of RA in genetically susceptible individuals:
- Smoking: Tobacco smoke is one of the most significant environmental risk factors. It can alter immune function and increase the risk of RA, particularly in individuals with specific genetic markers.
- Infections: Some viral and bacterial infections have been proposed as potential triggers for RA, although the specific pathogens and their roles remain subjects of research. Examples include:
- Epstein-Barr virus (EBV)
- Parvovirus B19
- Other respiratory viruses
- Obesity: Excess body weight is linked to systemic inflammation, which can contribute to the onset and progression of RA.
- Occupational Exposures: Certain jobs that expose individuals to silica dust, asbestos, or other chemicals may increase the risk of developing RA.
3. Hormonal Factors
- Gender: RA is more common in women than in men, indicating that hormonal factors may influence the disease. The onset often occurs during reproductive years, suggesting a potential link to hormonal changes.
- Pregnancy and Menopause: Some women may experience changes in RA symptoms during pregnancy or menopause, highlighting the role hormones may play in disease activity.
4. Immune System Dysfunction
- Autoimmunity: RA is classified as an autoimmune disease, where the immune system mistakenly attacks healthy joint tissues. This immune response is likely triggered by a combination of genetic predisposition and environmental factors.
- Inflammatory Cytokines: The disease process involves the release of inflammatory cytokines (e.g., tumor necrosis factor-alpha, interleukins) that promote inflammation and joint damage.
5. Other Contributing Factors
- Age: RA can occur at any age but is most commonly diagnosed in middle-aged individuals, typically between 30 and 60 years old.
- Vitamin D Deficiency: Some studies suggest that low levels of vitamin D may be associated with an increased risk of developing RA, possibly due to its role in immune function.
While the precise causes of rheumatoid arthritis are still being studied, a multifactorial approach encompassing genetic, environmental, hormonal, and immunological factors provides a comprehensive understanding of the condition. Recognizing these risk factors can lead to better prevention strategies and early intervention, potentially reducing the severity and progression of the disease. If you have concerns about RA or are experiencing symptoms, consulting a healthcare provider for evaluation and guidance is essential.
Diagnosis of Rheumatoid Arthritis
Diagnosing rheumatoid arthritis (RA) involves a comprehensive approach that includes a thorough medical history, physical examination, laboratory tests, and imaging studies. Early diagnosis is crucial for effective management and to prevent joint damage. Here’s a detailed overview of the diagnostic process:
1. Medical History
- Symptom Inquiry: The doctor will ask about the duration and nature of symptoms, including joint pain, stiffness, swelling, and any systemic symptoms like fatigue or fever.
- Family History: A detailed family history of autoimmune diseases or RA can provide insights into genetic predisposition.
- Lifestyle Factors: Information about smoking, diet, and physical activity may help identify risk factors.
2. Physical Examination
- Joint Assessment: The physician will examine affected joints for swelling, tenderness, warmth, and range of motion. They typically assess both the affected joints and those that are not symptomatic to determine symmetrical involvement.
- Extra-Articular Signs: The doctor will look for signs outside the joints, such as rheumatoid nodules, skin rashes, or signs of systemic involvement (e.g., lung or heart issues).
3. Laboratory Tests
Several blood tests can help confirm the diagnosis of RA and assess disease activity:
- Rheumatoid Factor (RF): This antibody is present in many individuals with RA, but it can also appear in other diseases. A positive RF test alone is not sufficient for diagnosis.
- Anti-Citrullinated Protein Antibody (ACPA): More specific for RA, the presence of ACPA is a strong indicator of the disease, even in the absence of RF.
- Erythrocyte Sedimentation Rate (ESR): This test measures the level of inflammation in the body. Elevated ESR levels can indicate active inflammation, but they are not specific to RA.
- C-Reactive Protein (CRP): Similar to ESR, CRP levels rise in response to inflammation and can help monitor disease activity.
- Complete Blood Count (CBC): A CBC can help detect anemia or other blood-related issues that might arise with RA.
4. Imaging Studies
Imaging techniques play a critical role in diagnosing and assessing the severity of RA:
- X-rays: Initial X-rays can help visualize joint damage, such as erosion of bone and changes in joint space. They may be used to monitor disease progression over time.
- Ultrasound: This non-invasive imaging method can detect inflammation in joints and assess soft tissue changes. It’s particularly useful for visualizing synovitis (inflammation of the synovial membrane).
- Magnetic Resonance Imaging (MRI): MRI is more sensitive than X-rays and can provide detailed images of both bone and soft tissues. It can help identify early signs of joint damage and inflammation.
5. Criteria for Diagnosis
The American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR) have established criteria for diagnosing RA, which include:
- Joint Involvement: Number and location of joints affected.
- Serology: Results of RF and ACPA tests.
- Acute Phase Reactants: Levels of CRP and ESR.
- Symptom Duration: Symptoms lasting more than six weeks.
A total score based on these criteria can help classify the likelihood of RA and guide diagnosis.
6. Differential Diagnosis
It’s important to distinguish RA from other types of arthritis and related conditions, including:
- Osteoarthritis
- Psoriatic arthritis
- Ankylosing spondylitis
- Gout
- Systemic lupus erythematosus
A thorough diagnostic process helps ensure that RA is correctly identified, enabling appropriate treatment and management.
The diagnosis of rheumatoid arthritis is a multifaceted process that combines clinical evaluation, laboratory tests, and imaging studies. Early and accurate diagnosis is essential to manage symptoms effectively, prevent joint damage, and improve the overall quality of life for those affected. If you suspect you may have RA, consult a healthcare professional for a comprehensive evaluation and tailored treatment plan.
Treatment of Rheumatoid Arthritis
While there is no cure for rheumatoid arthritis (RA), various treatment options are available to manage symptoms, reduce inflammation, slow disease progression, and improve the quality of life. The treatment plan is often personalized and may involve a combination of medications, lifestyle changes, physical therapy, and, in some cases, surgery.
1. Medications
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
- Function: These drugs help reduce pain and inflammation.
- Examples: Ibuprofen, naproxen, and diclofenac.
- Considerations: Long-term use can lead to gastrointestinal issues and cardiovascular risks, so they should be used cautiously.
Corticosteroids
- Function: These medications quickly reduce inflammation and suppress the immune response.
- Examples: Prednisone and methylprednisolone.
- Usage: Often used during flare-ups or when other medications are not effective.
- Side Effects: Long-term use can lead to weight gain, osteoporosis, and increased risk of infections.
Disease-Modifying Antirheumatic Drugs (DMARDs)
- Function: These drugs slow the progression of RA and prevent joint damage.
- Examples:
- Methotrexate: Often the first choice for RA treatment, it reduces inflammation and prevents joint damage.
- Sulfasalazine and Leflunomide: Other options that may be used based on individual response and tolerability.
- Monitoring: Regular blood tests are often required to monitor for side effects.
Biologics
- Function: Target specific components of the immune system involved in the inflammatory process.
- Examples:
- TNF Inhibitors: Etanercept, infliximab, and adalimumab.
- Non-TNF Biologics: Abatacept and rituximab.
- Usage: Typically used when traditional DMARDs are insufficient or not tolerated.
- Considerations: May increase the risk of infections and require monitoring for side effects.
Janus Kinase (JAK) Inhibitors
- Function: A newer class of medications that target specific pathways in the immune response.
- Examples: Tofacitinib and baricitinib.
- Usage: Often considered when other treatments have failed.
- Monitoring: Regular blood tests are needed to assess liver function and blood cell counts.
2. Physical and Occupational Therapy
- Physical Therapy: A physical therapist can create an exercise program to improve flexibility, strength, and overall joint function. This may include:
- Range-of-motion exercises: To maintain joint flexibility.
- Strength training: To improve muscle strength around affected joints.
- Low-impact aerobic exercises: To promote cardiovascular health without putting undue stress on the joints.
- Occupational Therapy: An occupational therapist can help with strategies and tools to perform daily activities with less pain, including adaptive devices for the kitchen, bathroom, or workplace.
3. Lifestyle Modifications
Diet
- Anti-Inflammatory Foods: A diet rich in fruits, vegetables, whole grains, and omega-3 fatty acids (found in fish and flaxseed) may help reduce inflammation.
- Avoiding Triggers: Some people find that certain foods exacerbate their symptoms, and keeping a food diary can help identify these triggers.
Exercise
- Regular Activity: Engaging in regular, low-impact exercise can improve joint function, reduce stiffness, and enhance overall health.
- Flexibility and Balance Training: Activities like yoga or tai chi can improve flexibility and reduce stress.
Weight Management
- Healthy Weight: Maintaining a healthy weight can reduce stress on the joints, particularly weight-bearing joints like the knees and hips.
4. Alternative Therapies
While not replacements for conventional treatments, some people find relief from RA symptoms through complementary approaches:
- Acupuncture: May help reduce pain and improve function in some individuals.
- Massage Therapy: Can help relieve muscle tension and improve circulation.
- Mind-Body Techniques: Practices such as meditation, mindfulness, and relaxation techniques can help manage stress and improve emotional well-being.
5. Surgery
In cases where joint damage is severe and other treatments have not provided adequate relief, surgical options may be considered:
- Synovectomy: Removal of the inflamed synovial membrane to reduce inflammation and pain.
- Joint Replacement: Replacement of severely damaged joints (e.g., knees, hips) can restore function and reduce pain.
- Arthrodesis: Fusion of bones in a joint to stabilize and alleviate pain.
Managing rheumatoid arthritis requires a comprehensive and individualized approach that combines medication, physical therapy, lifestyle changes, and possibly surgery. Regular follow-up with healthcare providers is essential to monitor disease progression, adjust treatment plans as needed, and ensure the best possible outcomes. If you suspect you have RA or are experiencing symptoms, consulting a rheumatologist or healthcare professional is vital for appropriate diagnosis and management.
Living with Rheumatoid Arthritis
Living with rheumatoid arthritis (RA) can present daily challenges, but many people successfully manage their symptoms and lead fulfilling lives. Understanding the condition and implementing effective strategies can make a significant difference. Here’s a detailed overview of how to navigate life with RA.
1. Managing Symptoms
Pain Management
- Medications: Regularly take prescribed medications, including NSAIDs, DMARDs, or biologics, as directed by your healthcare provider.
- Heat and Cold Therapy: Applying heat can relax tense muscles and improve blood flow, while cold packs can numb acute pain and reduce inflammation.
- Topical Treatments: Over-the-counter creams or ointments that contain analgesics or capsaicin may provide localized relief.
Recognizing Flare-Ups
- Identify Triggers: Keep a symptom diary to track activities, stress levels, diet, and other factors that may trigger flare-ups.
- Early Intervention: If you notice early signs of a flare (increased pain, stiffness), consult your doctor about adjusting your treatment plan promptly.
2. Psychological and Emotional Well-Being
Mental Health Support
- Therapy: Consider counseling or therapy to address the emotional challenges of living with a chronic condition. Cognitive-behavioral therapy (CBT) can be particularly effective.
- Support Groups: Joining a local or online support group can provide a sense of community, allowing you to share experiences and coping strategies.
Stress Management
- Mindfulness and Relaxation Techniques: Practices like yoga, meditation, and deep-breathing exercises can reduce stress and promote emotional well-being.
- Hobbies and Interests: Engage in activities you enjoy to boost your mood and distract from pain.
3. Staying Active
Exercise
- Regular Physical Activity: Engage in low-impact exercises such as walking, swimming, or cycling to maintain joint function and overall fitness.
- Strength Training: Incorporate gentle strength training to build muscle support around joints.
- Flexibility and Stretching: Include stretching routines to enhance flexibility and reduce stiffness.
4. Diet and Nutrition
Anti-Inflammatory Diet
- Emphasize Whole Foods: Focus on a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats (e.g., olive oil, nuts).
- Omega-3 Fatty Acids: Include sources of omega-3s, such as fatty fish (salmon, sardines) or flaxseed, which may help reduce inflammation.
- Hydration: Drink plenty of water to stay hydrated and support overall health.
Monitoring Food Sensitivities
- Food Diary: Keeping a food diary can help identify foods that may exacerbate symptoms. Common triggers include processed foods, sugar, and gluten in some individuals.
5. Work and Daily Life
Communicating with Employers
- Disclose Needs: If comfortable, communicate with your employer about your condition. Discuss any accommodations that may help you perform your job effectively.
- Flexible Work Arrangements: Consider negotiating for flexible hours or the option to work from home when necessary.
Time Management
- Prioritize Tasks: Focus on completing essential tasks when you have the most energy. Break larger tasks into manageable steps.
- Rest and Recovery: Schedule regular breaks and listen to your body’s signals. Allow yourself time to rest, especially during flare-ups.
6. Regular Medical Care
Routine Check-Ups
- Regular Appointments: Schedule routine visits with your rheumatologist to monitor disease activity and adjust treatment as needed.
- Screening for Complications: Regular screenings for conditions associated with RA, such as cardiovascular disease and osteoporosis, are important for overall health.
7. Support Networks
Building a Support System
- Family and Friends: Educate your loved ones about RA so they can provide better support and understanding.
- Healthcare Team: Establish a strong relationship with your healthcare providers, including your rheumatologist, primary care physician, physical therapist, and dietitian.
Living with rheumatoid arthritis requires a proactive approach that encompasses physical health, mental well-being, and lifestyle adjustments. By understanding your condition, managing symptoms effectively, and building a support network, you can enhance your quality of life and maintain a fulfilling daily routine. Regular communication with healthcare providers and loved ones is crucial for navigating the challenges of RA and achieving the best possible outcomes. If you have specific concerns or questions about living with RA, don’t hesitate to reach out to a healthcare professional for guidance.

Rheumatoid arthritis is a complex disease that requires a comprehensive approach to treatment and management. Early diagnosis and a tailored treatment plan can significantly improve the quality of life for those affected. If you suspect you have RA or are experiencing joint pain and inflammation, consult a healthcare professional for a thorough evaluation.