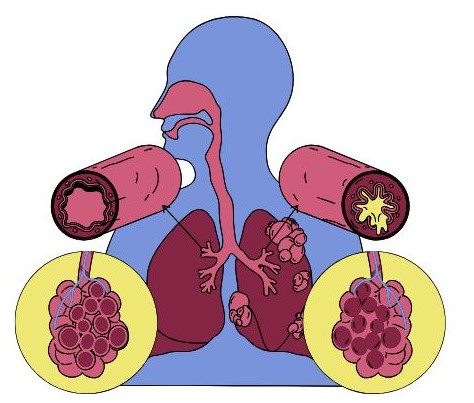
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease that causes breathing difficulties. It encompasses a group of conditions, primarily chronic bronchitis and emphysema, that obstruct airflow in the lungs, leading to reduced oxygen exchange. COPD is a major cause of morbidity and mortality worldwide and significantly impacts the quality of life for those affected. This article provides a detailed overview of COPD, including its symptoms, causes, diagnosis, and management strategies.
What is COPD?
COPD is characterized by long-term respiratory symptoms and airflow limitation due to airway obstruction. It is primarily caused by inhalation of harmful substances, most commonly cigarette smoke, but also includes exposure to pollutants and occupational hazards.
Key Features
- Chronic Bronchitis: Inflammation of the bronchial tubes, resulting in increased mucus production, chronic cough, and difficulty breathing.
- Emphysema: Damage to the alveoli (air sacs) in the lungs, leading to reduced surface area for gas exchange and difficulty in exhaling air.
Symptoms of COPD
- Chronic Cough
- Description: A persistent cough that lasts for three months or longer, often occurring daily.
- Characteristics: Initially may be dry but often progresses to a productive cough that produces mucus. This cough is typically worse in the mornings and can become more pronounced with physical activity or exposure to irritants.
- Shortness of Breath (Dyspnea)
- Description: Difficulty breathing, particularly during physical exertion.
- Characteristics: Early stages may only involve shortness of breath during activities like climbing stairs or exercising. As the disease progresses, it can occur even at rest or with minimal exertion, significantly impacting daily activities.
- Wheezing
- Description: A high-pitched whistling sound when breathing, especially during exhalation.
- Characteristics: Wheezing may become more pronounced during physical activity or during respiratory infections, indicating airway constriction.
- Chest Tightness
- Description: A feeling of pressure or tightness in the chest, often described as a band-like sensation.
- Characteristics: This can lead to discomfort and anxiety, as the individual may feel unable to take a deep breath.
- Increased Mucus Production
- Description: Overproduction of mucus due to inflammation in the airways.
- Characteristics: Mucus may be clear, yellow, or greenish and can lead to frequent throat clearing or coughing to expel it. This symptom is particularly prominent in chronic bronchitis.
- Frequent Respiratory Infections
- Description: Individuals with COPD are more susceptible to infections such as colds, flu, and pneumonia.
- Characteristics: These infections can exacerbate symptoms and lead to significant flare-ups, making management more challenging.
- Fatigue
- Description: Chronic tiredness and lack of energy.
- Characteristics: Fatigue in COPD patients can result from the increased effort required to breathe, reduced physical activity, and poor sleep quality. This can affect daily functioning and quality of life.
- Cyanosis
- Description: A bluish tint to the skin, lips, or fingernails, indicating low oxygen levels in the blood.
- Characteristics: This symptom usually occurs in more advanced stages of COPD and signifies a need for medical intervention.
- Weight Loss
- Description: Unintentional weight loss may occur in more severe cases.
- Characteristics: This can result from increased metabolic demands due to breathing difficulties or a decreased appetite due to respiratory symptoms.
- Swelling in the Ankles, Feet, or Legs
- Description: Edema may develop due to heart complications associated with severe COPD.
- Characteristics: This can occur when the heart struggles to pump effectively, often referred to as cor pulmonale, which is a complication of advanced COPD.
- Depression and Anxiety
- Description: Many individuals with COPD experience emotional health challenges.
- Characteristics: The limitations imposed by the disease can lead to feelings of isolation, sadness, and anxiety about health and future activities.
Progression of Symptoms
- Early Stages: Symptoms may be mild and not significantly interfere with daily activities. A chronic cough and occasional shortness of breath are common.
- Moderate Stages: As the disease progresses, symptoms become more pronounced. Shortness of breath may occur with everyday activities, and exacerbations may lead to increased coughing and mucus production.
- Severe Stages: In advanced COPD, individuals may experience persistent breathlessness, significant fatigue, and a marked decrease in physical activity. Frequent hospitalizations may occur due to exacerbations.
Understanding the diverse symptoms of COPD is crucial for early recognition and effective management of the disease. If you or someone you know is experiencing these symptoms, it’s important to seek medical advice for proper diagnosis and treatment. Early intervention can significantly improve quality of life and slow the progression of the disease.
Causes and Risk Factors
Primary Causes
- Tobacco Smoke: The leading cause of COPD, accounting for the majority of cases. Both active smoking and exposure to secondhand smoke are significant risk factors.
- Air Pollution: Long-term exposure to indoor and outdoor air pollutants, including dust, chemicals, and fumes, can contribute to COPD development.
- Occupational Exposures: Certain jobs that involve exposure to harmful dusts and chemicals can increase the risk of COPD.
- Genetic Factors: A rare genetic disorder known as Alpha-1 Antitrypsin Deficiency can lead to early onset emphysema.
Risk Factors
- Age: COPD is more common in individuals over 40 years old.
- Gender: Historically, more men have been diagnosed with COPD, but the gap is closing as more women smoke.
- Family History: A family history of lung diseases can increase the risk.
- Socioeconomic Status: Individuals with lower socioeconomic status may have increased exposure to risk factors and limited access to healthcare.
Diagnosis of COPD
Diagnosing COPD typically involves several steps:
1. Medical History and Symptoms
- Symptom Assessment: Healthcare providers will evaluate the patient’s symptoms, medical history, and any exposure to risk factors.
- Smoking History: A thorough history of smoking and exposure to pollutants is essential.
2. Physical Examination
- Respiratory Exam: A physical examination may reveal wheezing, prolonged expiration, and signs of respiratory distress.
3. Diagnostic Tests
- Spirometry: The most important test for diagnosing COPD, spirometry measures lung function by assessing how much air a person can exhale and how quickly. A reduced Forced Expiratory Volume (FEV1) to Forced Vital Capacity (FVC) ratio indicates airflow limitation.
- Chest X-ray or CT Scan: Imaging studies may be used to evaluate lung structure and rule out other conditions.
- Arterial Blood Gas Analysis: This test measures oxygen and carbon dioxide levels in the blood, providing information about lung function.
Management and Treatment
While there is no cure for COPD, effective management can significantly improve quality of life and reduce symptoms. Treatment strategies include:
1. Lifestyle Modifications
- Smoking Cessation: The most crucial step for individuals with COPD. Quitting smoking can slow disease progression and improve lung function.
- Avoiding Pollutants: Reducing exposure to indoor and outdoor pollutants can help manage symptoms.
2. Medications
- Bronchodilators: These medications help open airways and improve breathing. They can be short-acting (used as needed) or long-acting (taken regularly).
- Inhaled Corticosteroids: These may be prescribed to reduce inflammation in the airways and decrease the frequency of exacerbations.
- Combination Inhalers: Combining bronchodilators with inhaled corticosteroids can provide enhanced benefits.
- Phosphodiesterase-4 Inhibitors: These medications can reduce inflammation and relax the airways in more severe cases.
3. Pulmonary Rehabilitation
- Structured Programs: These programs combine education, exercise training, nutrition advice, and counseling to help individuals manage COPD more effectively.
- Exercise Training: Regular physical activity can improve overall fitness, reduce symptoms, and enhance the ability to perform daily activities.
4. Oxygen Therapy
- Supplemental Oxygen: For individuals with low blood oxygen levels, oxygen therapy can help improve oxygenation and reduce symptoms of breathlessness.
5. Vaccinations
- Preventive Measures: Vaccinations for influenza and pneumonia are recommended to prevent respiratory infections, which can exacerbate COPD symptoms.
6. Surgical Options
- Lung Volume Reduction Surgery: In selected patients with severe emphysema, this surgery can remove damaged lung tissue to improve breathing.
- Lung Transplant: In advanced cases, lung transplantation may be considered for eligible candidates.
Living with COPD
1. Understanding Your Condition
- Education: Learning about COPD, its symptoms, and management options is crucial. Understanding how the disease progresses and what triggers symptoms can help you take proactive steps in managing your health.
- Tracking Symptoms: Keeping a journal of your symptoms, medication use, and any changes can help you and your healthcare provider make informed decisions about your treatment plan.
2. Symptom Management Strategies
- Breathing Techniques:
- Pursed-Lip Breathing: Inhale through your nose and exhale slowly through pursed lips. This technique helps keep airways open longer and can reduce shortness of breath.
- Diaphragmatic Breathing: Focus on using your diaphragm rather than your chest to breathe. This can improve lung efficiency and reduce fatigue.
- Medication Adherence:
- Inhalers and Medications: Use prescribed bronchodilators and corticosteroids as directed. Setting reminders or using pill organizers can help ensure you take medications on time.
- Rescue Inhalers: Keep a rescue inhaler handy for quick relief of acute symptoms.
3. Lifestyle Modifications
- Exercise:
- Regular Physical Activity: Engage in low-impact exercises, such as walking, swimming, or cycling, to improve lung function and overall fitness. A pulmonary rehabilitation program can provide guided exercise tailored to your abilities.
- Strength Training: Building muscle strength can help improve endurance and decrease fatigue.
- Nutrition:
- Healthy Eating: Focus on a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Proper nutrition can help maintain energy levels and support overall health.
- Hydration: Staying hydrated helps keep mucus thin and easier to clear from the lungs.
- Sleep Hygiene:
- Quality Sleep: Prioritize good sleep practices, such as maintaining a regular sleep schedule, creating a comfortable sleep environment, and avoiding stimulants before bedtime. Poor sleep can exacerbate fatigue and respiratory symptoms.
4. Managing Exacerbations
- Recognizing Triggers: Identify factors that may worsen symptoms, such as allergens, air pollution, respiratory infections, and weather changes.
- Action Plan: Work with your healthcare provider to create a personalized action plan for managing exacerbations. This plan should include steps to take when symptoms worsen and when to seek medical help.
5. Oxygen Therapy
- Supplemental Oxygen: If prescribed, use supplemental oxygen as directed. This can help improve oxygen levels in the blood and alleviate shortness of breath.
- Portable Options: Explore portable oxygen solutions to maintain mobility and continue participating in daily activities.
6. Emotional and Mental Health Support
- Mental Health Awareness: Many individuals with COPD experience anxiety, depression, or feelings of isolation. Recognizing these emotions is essential for overall well-being.
- Counseling and Support Groups: Consider talking to a therapist or joining support groups where you can share experiences and strategies with others facing similar challenges.
7. Seeking Professional Help
- Regular Check-ups: Schedule routine appointments with your healthcare provider to monitor lung function and adjust treatment as necessary.
- Vaccinations: Stay up-to-date with vaccinations for influenza and pneumonia to prevent respiratory infections that can exacerbate COPD symptoms.
8. Creating a Support Network
- Family and Friends: Communicate openly with family and friends about your condition. Educating them on your needs can foster understanding and support.
- Caregiver Support: If you have a caregiver, involving them in your healthcare discussions can improve your management strategies and provide additional support.
9. Home Environment Adjustments
- Air Quality: Maintain good indoor air quality by using air purifiers, keeping windows closed during high pollen days, and avoiding smoking indoors.
- Avoiding Triggers: Minimize exposure to strong odors, dust, and pet dander, which can trigger symptoms.
Living with COPD requires a multifaceted approach that includes effective symptom management, lifestyle modifications, and emotional support. By understanding the condition, adhering to treatment plans, and maintaining an active and healthy lifestyle, individuals with COPD can significantly improve their quality of life. If you or someone you know is living with COPD, remember that proactive management and support are key to navigating daily challenges and maintaining well-being.

Chronic Obstructive Pulmonary Disease (COPD) is a significant public health issue that requires early recognition and comprehensive management. While it poses challenges, understanding the disease and implementing effective treatment strategies can help individuals lead more active and fulfilling lives. If you or someone you know is experiencing symptoms of COPD, seeking medical advice is essential for diagnosis and appropriate management.